Useful information for patients and interested parties
Things to know about Long COVID
What is Long COVID and how is it different from Post COVID?
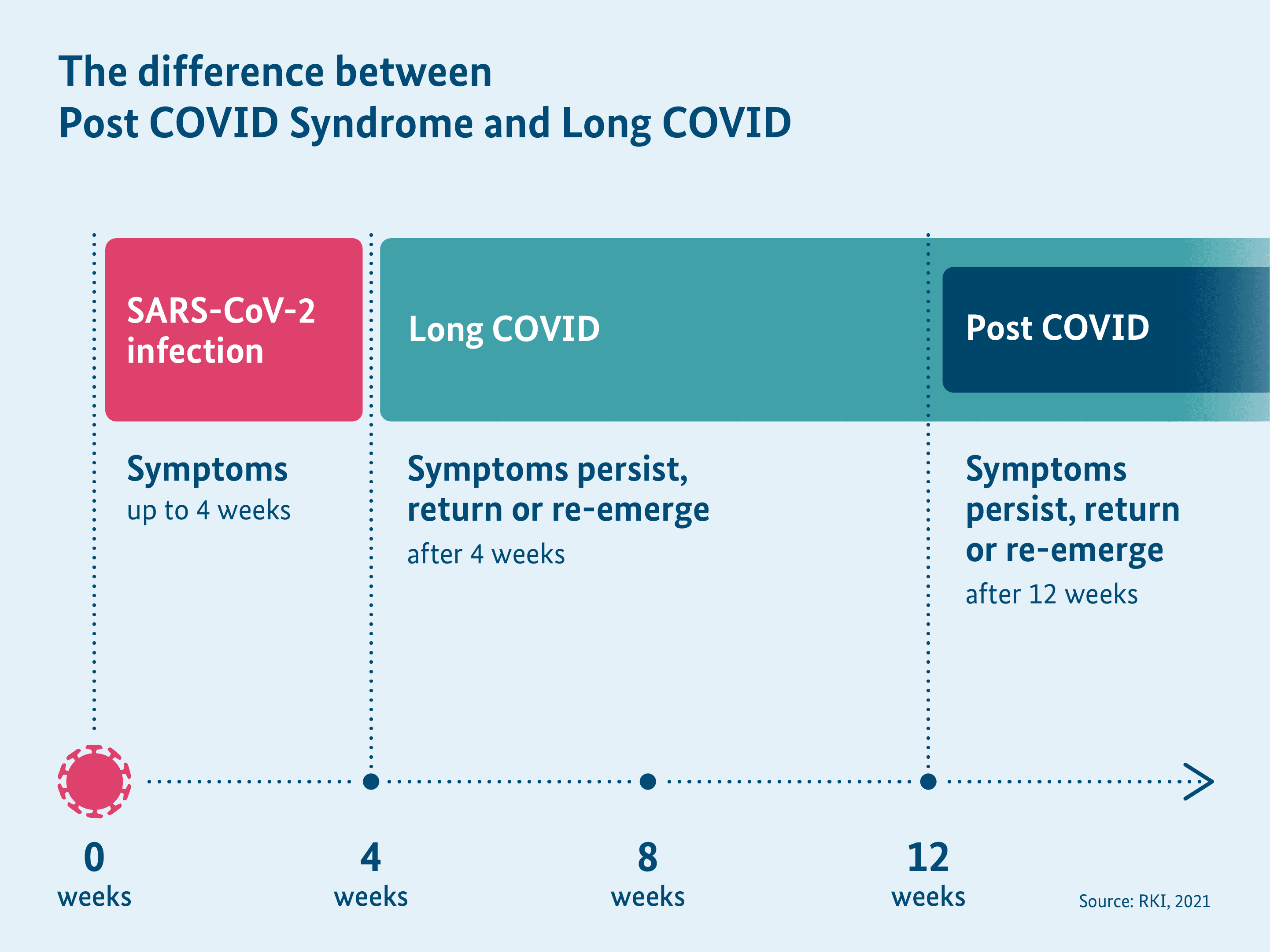
The general long-term health effects after a Corona virus SARS-CoV-2 infection are called Long COVID. A distinction is made between Long COVID and Post COVID in medicine and science depending on the duration of the symptoms.
The term Long COVID covers long-term, health problems, which last beyond the acute illness phase of 4 weeks after the infection. The symptoms can also arise already during the COVID-19 illness and last or recur. They can even reappear as late as several weeks after the Corona virus infection. Long COVID also manifests by worsening a pre-existing illness. Overall, long-term health symptoms may arise even after an initially mild or asymptomatic course of illness. Meanwhile, the term PASC is also used worldwide for such long-term effects after a Corona virus infection. PASC is the English abbreviation for “post-acute sequelae of COVID-19”. The American RECOVER Initiative has developed a case definition for PASC in 2023.
Post COVID refers to symptoms in adults, which are still present or arise newly or again even 12 weeks after a Corona virus infection. In children and adolescents, it is considered Post COVID after 8 weeks itself. The symptoms last for at least 2 months and cannot be explained otherwise. Furthermore, the long haulers are generally affected in everyday life, says the definition of World Health Organisation (WHO).
As an umbrella term, Long COVID or PASC covers all long-term symptoms, which are present longer than 4 weeks after a Corona virus infection and thus also covers Post COVID.
The currently available scientific studies do not always use the definitions for Long COVID and Post COVID homogenously. Therefore, an allocation to Long COVID and Post COVID cannot always be made selectively.
This website homogenously talks of Long COVID. By this, we mean symptoms in the entire period from 4 weeks after the Corona virus infection.
Last update: December 2024
Why and how does Long COVID come into being?
How and why exactly Long COVID occurs is still not sufficiently clear at present. In principle, long-term health effects can also occur after many other infections. For example, such sequelae are known even after a viral flu (influenza) or EBV infection (“glandular disease”). It therefore remains important to investigate the underlying causes in detail. Research into this will continue. However, there is widespread scientific agreement that there are different mechanisms of disease development for Long COVID, and that Long COVID is not a consistent disease pattern.
The large number of different symptoms of Long COVID can possibly be explained by how the coronavirus enters the human body: The virus enters the body through certain receptor sites, i.e. the so-called ‘ACE2 receptors’. These receptor sites are present in many tissues and organs in the human body. That could explain why the symptoms of Long COVID are so varied and affect different organs. ACE2 receptors are also present on the inside of blood vessels. If the Corona virus binds to the ACE2 receptors, the virus can cause inflammations and activate the immune system. Some theories that could be relevant are being researched and discussed at present.
Here is an overview of the scientific theories on the origin of Long COVID:
- One theory is that Long COVID is the result of a so-called auto-immune reaction. In auto-immune reactions, the immune system directs itself against the body’s own cells. Normally, the immune system fights only the changed cells in the body as well as pathogens and foreign substances. After a COVID-19 illness, the immune system is significantly activated. According to the theory, the immune system then also attacks its own body cells after a COVID-19 illness. It is also suggested by some researchers that Long COVID can trigger auto-immune diseases or accelerate their development. The fact that certain antibodies, the so-called autoantibodies, were found in multiple studies in some Long COVID patients supports this theory. Autoantibodies are antibodies that act against autologous structures.
- Another theory hypothesises that Long COVID arises due to a prolonged inflammation in the body. According to this theory, the Corona virus activates the immune system for the long term and keeps it in a kind of alertness. That could lead to prolonged inflammations in organs such as the kidneys, lungs, or brain. For example, inflammations in the small blood vessels in various organs have been described. These blood vessels are important to supply the organs with sufficient oxygen.
- Some researchers found that residues of the virus can remain in the body even weeks to months after a Corona virus infection. Components of the virus have been found, for example, in the cardiovascular system, brain, muscles, lungs, liver, and in some other organs. It is conceivable that there continue to be symptoms and inflammations in the body due to these virus residues. The immune system then possibly remains activated due to the virus residues in the body.
- According to another theory, other viruses that survive in the body are reactivated by a dysregulated immune system. Some viruses such as Epstein Barr virus (EBV, pathogen of “glandular fever”) or other herpes viruses remain in the body for life following an infection but normally do not cause any damage. But they can be reactivated in the wake of COVID-19 and could thus favour the development of Long COVID. Researchers have been suspecting for some time now that EBV can aggravate the symptoms of other illnesses (for example, symptoms of autoimmune diseases or ME/CFS).
- Apart from that, slightest blood clots in blood vessels seem to be involved in the development of Long COVID, the so-called microclots. These blood clots could result in very small blood vessels not being properly supplied with blood (disrupted microcirculation). Such a disrupted blood circulation can explain many of the symptoms in Long COVID to some extent.
- In addition, the energy metabolism in mitochondria appeared to be impaired in some long haulers. Mitochondria are a part of the somatic cells and are also called the “powerhouse” of the cells because they make energy available. This theory could explain, why the symptoms worsen in some long haulers already after slight exertion (so-called “stress intolerance” or “Post exertional malaise” abbreviated PEM).
- A disturbed gut flora due to changes in the bacterial composition in the intestine could be involved in the development of Long COVID.
- Apart from that, it is discussed whether a disturbed brain stem or vagus nerve function is involved in the development of Long COVID. The vagus nerve regulates many different involuntary processes in the body, for example, heartbeat and digestion.
Multiple mechanisms are likely to be involved in the development of Long COVID. None of the theories have a conclusive scientific consensus until now and the research on the possible causes continues to go on.
Sources:
https://www.nature.com/articles/s41577-023-00904-7
https://pmc.ncbi.nlm.nih.gov/articles/PMC10408714/
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1428645/full
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(24)00211-1/fulltext
https://www.mdpi.com/2079-9721/12/5/95
https://www.nature.com/articles/s41591-022-01810-6
https://www.nature.com/articles/s41579-022-00846-2
https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2020.594495/full
https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.698169/full
https://www.bmj.com/content/374/bmj.n1648
https://www.mdpi.com/1422-0067/24/19/14822
https://www.nature.com/articles/s41467-023-44432-3
https://www.nature.com/articles/s41380-022-01836-9
https://www.aerzteblatt.de/archiv/229207/Post-COVID-Syndrom
https://www.the-scientist.com/news-opinion/long-covid-likely-doesn-t-have-just-one-cause-70559
https://www.nature.com/articles/s41590-021-01113-x
https://cardiab.biomedcentral.com/articles/10.1186/s12933-021-01359-7
https://www.nature.com/articles/s41575-022-00698-4
https://www.cell.com/cell/fulltext/S0092-8674(22)00072-1
https://insight.jci.org/articles/view/152346
https://www.ingentaconnect.com/content/ocean/aap/2022/00000043/00000003/art00003
Further information:
Last update: December 2024
How common is Long COVID?
It cannot be conclusively said yet as to how many people have been affected by Long COVID. The previous studies have differing results. An accurate estimation is therefore difficult, among other things because the studies were conducted at different points in time. The various virus variants make a difference here. So compared to the earlier virus variants, Long COVID appears to occur more rarely in people, who were infected by the Omicron variant. Apart from that, the number of vaccinated people has risen. Overall, the risk for Long COVID has decreased in the past years.
Other factors also lead to differing results regarding the frequency of Long COVID. In part, the studies used different definitions for the long-term health effects of COVID-19. Some studies refer to all long-term effects, which persist longer than 4 weeks after a Corona virus infection, corresponding to the definition of “Long COVID”. Other studies refer to only long-term effects, which continue longer than 12 weeks after an infection, corresponding to the definition of “Post COVID”. Apart from that, the studies sometimes consider different symptoms and various impacts such as pre-existing conditions.
Which people participated in the respective study is also something that matters. The explanation for this is: Numerous factors influence whether a person will contract Long COVID. These include age, sex, pre-existing health risks such as pre-existing conditions and, how severely a person contracted the COVID-19 infection. Thus, Long COVID is considerably more common if you examine people who had to be treated for COVID-19 in a hospital or even in an intensive care unit.
Furthermore, different research methods make the evaluation of the studies difficult. For example, it is important to compare people who have had Corona virus infection with other people, who have not been infected by the Corona virus until now. This method is significant because the possible physical and psychological symptoms after a Corona virus infection can also have other causes. These include, for example, general strains due to the pandemic, which have to be demarcated from the long-term health effects after a Corona virus infection. In some studies, an additional comparison is made with people who had fallen ill with a viral flu (influenza) before the COVID-19 pandemic. The results until now are not uniform: Some studies suggest that long-term health effects after a Corona virus infection seemed to arise overall more frequently and last longer than, for example, after a viral flu. In other studies no difference in the long-term health effects was found after other viral infections.
For more information, please also read the answers to the questions ‘How do different variants of the SARS-CoV-2 coronavirus affect the risk of Long COVID?’ and ‘What factors influence the personal risk of contracting Long COVID?’.
Sources:
https://www.nejm.org/doi/10.1056/NEJMoa2403211
https://bmjpublichealth.bmj.com/content/1/1/e000060
https://www.nature.com/articles/s41579-022-00846-2
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2821459
https://academic.oup.com/cid/article/77/2/194/7076063
https://academic.oup.com/ofid/article/10/7/ofad233/7150886
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)01214-4/fulltext
https://www.nature.com/articles/s41467-022-33415-5
https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003773
https://www.bmj.com/content/371/bmj.m4677
https://www.nature.com/articles/s41467-022-30836-0
https://www.bmj.com/content/379/bmj-2022-071050
https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofac333/6628648
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00381-9/fulltext
https://www.nature.com/articles/s41586-021-03553-9
Further information:
Last update: December 2024
How do different variants of the SARS-CoV-2 coronavirus affect the risk of Long COVID?
There are increasing indications that the risk of developing Long COVID differs depending on the virus variant. Accordingly, an infection by the Omicron variant appears to lead to symptoms of Long COVID less often than the earlier variants. Individual studies also provide initial indications that Long COVID symptoms after an infection by the Omicron variant are less severe and the patients recover faster. However, the number of studies on this topic is limited until now and the results are inconsistent. Therefore, a conclusive evaluation still cannot be done.
Sources:
https://www.cell.com/heliyon/fulltext/S2405-8440(24)04972-7
https://link.springer.com/article/10.1007/s15010-024-02270-5
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0302408
https://www.thelancet.com/journals/landig/article/PIIS2589-7500(23)00056-0/fulltext
https://academic.oup.com/cid/article/77/2/194/7076063
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0281429
https://www.mdpi.com/1999-4915/14/12/2629
https://www.mdpi.com/1660-4601/19/23/16010
https://www.nature.com/articles/s41467-022-35240-2
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
Further information:
Last update: December 2024
What factors influence a person’s risk of developing Long COVID?
To date, various potential factors that could pose a risk for or protection against Long COVID have been identified. Many studies agree that certain factors may be able to increase the risk of Long COVID.
Age and sex:
Younger adults appear to be affected more frequently than older people, children and adolescents. Additionally, according to the findings thus far, women are affected more often than men. As part of a review from the year 2023, the findings from 38 different studies with a total of 727,630 participants were examined. Researchers subsequently concluded that women were at higher risk of developing Long COVID than men.
Pre-existing health risks:
Besides age and sex, according to current scientific findings additional factors may increase the risk of developing Long COVID. These include pre-existing health risks such as smoking as well as various physical and mental conditions, for instance being overweight, asthma, chronic obstructive pulmonary disease (COPD), diabetes, coronary heart disease, anxiety and depression. Further risk factors potentially include certain connective tissue diseases and allergies.
Severe course of COVID-19 illness:
People are also at higher risk of developing Long COVID if they have had a severe case of COVID-19 and required hospitalisation for treatment. As part of a comprehensive review, people who had had severe COVID-19 were more than twice as likely to develop Long COVID as people as people who had only had mild COVID-19.
Repeated SARS-CoV-2 infections:
There are indications that each renewed SARS-CoV-2 infection (referred to as a re-infection) constitutes a risk factor for Long COVID. The state of knowledge is still limited, so there is still further need for research.
Protection through the COVID-19 vaccine
The COVID-19 vaccine indirectly provides protection against Long COVID by preventing infections and severe disease progressions. The results of various observational studies indicate a certain level of protection from the emergence of Long COVID following a breakthrough infection where someone is fully vaccinated against COVID-19 (with EU-approved vaccines or comparable). Due to the inconsistent definition and recording of the endpoint deemed “Long COVID” within these studies, it is not possible to make an evidence-based, conclusive statement regarding the extent and duration of this effect.
The Federal Centre for Health Education (BZgA) offers information regarding possible protective measures against the coronavirus. There you will find information on COVID-19 vaccination for children, adolescents and adults. Use the Corona-Impfcheck (coronavirus vaccination check) to get the latest vaccination recommendations. The latest vaccination recommendations by the Standing Committee on Vaccination (STIKO) as well as further information are available on the website of the Robert Koch Institute (RKI).
Should Long COVID patients receive a COVID-19 booster?
According to the RKI, at this point in time the STIKO has not made a separate vaccination recommendation for Long COVID patients to receive a yearly booster due to the very heterogeneous study data on COVID-19 vaccination among patients who already exhibit Long or Post COVID symptoms.
In order to prevent severe COVID-19 progressions, for certain risk groups the STIKO recommends an annual booster.
For further information on this topic, visit the RKI website.
Sources:
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2802877
https://www.nature.com/articles/s41579-022-00846-2
https://www.nejm.org/doi/10.1056/NEJMoa2403211
https://www.sciencedirect.com/science/article/pii/S0264410X23001342?via%3Dihub
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9905096/
https://academic.oup.com/jid/article/226/9/1593/6569364
https://www.nature.com/articles/s41581-022-00652-2
https://www.nature.com/articles/s41591-022-02051-3
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)00941-2/fulltext
https://www.cell.com/cell/fulltext/S0092-8674(22)00072-1
https://www.mdpi.com/2077-0383/11/24/7314
https://www.nature.com/articles/s41591-022-02051-3
https://pmc.ncbi.nlm.nih.gov/articles/PMC10633780/
https://linkinghub.elsevier.com/retrieve/pii/S0163-4453(24)00140-3
https://jamanetwork.com/journals/jama/fullarticle/2805540
https://pubmed.ncbi.nlm.nih.gov/36231717/
https://jamanetwork.com/journals/jama/fullarticle/2797443
https://www.impfen-info.de/impfempfehlungen/fuer-erwachsene/corona-schutzimpfung-bei-erwachsenen/
https://www.infektionsschutz.de/coronavirus/fragen-und-antworten/sich-und-andere-schuetzen/
Further information:
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0281429
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9905096/
https://www.nature.com/articles/s41579-022-00846-2
Last update: December 2024
Which symptoms can arise in Long COVID?
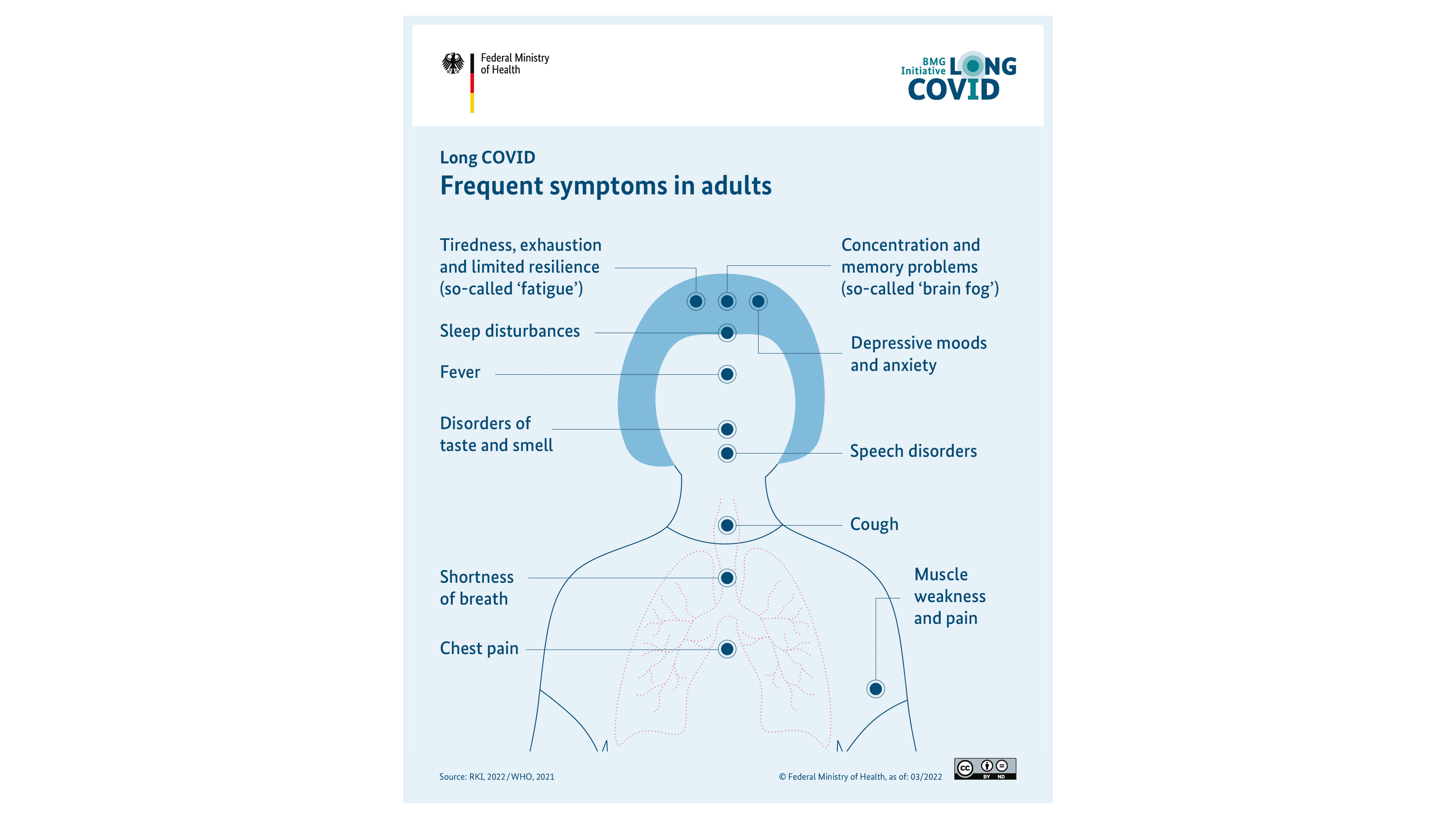
You can see various examples of frequent Long COVID symptoms in adults in this info-graphic.
According to the current state of knowledge, Long COVID is not a uniform clinical pattern. In the meanwhile, a number of Long COVID symptoms have been known. The symptoms arise individually or in combination. Additionally, the symptoms can fluctuate in their intensity. There can be times when you feel better and times when the symptoms worsen again.
Since some of the symptoms of Long COVID resemble one another, they are sometimes combined into so-called symptom complexes. The frequently arising symptom complexes are briefly explained below:
1. Fatigue and stress intolerance
An acute, prolonged weakness and exhaustion rank among most frequent symptoms in Long COVID. This is also called “fatigue”. Long haulers report, for instance, being exhausted especially quickly or needing extraordinary recovery time. However, breaks or sleeping rarely improve the symptoms or only for a short-term.
The fatigue is also accompanied by a so-called stress intolerance in part. This is also called PEM (Post Exertional Malaise). In a PEM, the symptoms can already worsen by a mild physical or mental exertion such as brisk walking or mental effort. It is also called as “Crash”. “Crash” means “collapse” or “hard setback”.
PEM is the most important feature of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome (ME/CFS). This illness is accompanied by acute exhaustion, PEM, mental problems and aches. The long haulers are often greatly restricted in their daily routine. According to researchers, ME/CFS can also arise in a potential progressive form of Long COVID. What exactly leads to this illness is presently under intensive research. It also arises as a consequence of other infectious diseases (also see the answer to the question “Are there overlaps between Long COVID and ME/CFS?”).
ME/CFS is frequently accompanied by a so-called “postural tachycardia syndrome” (POTS), which can also occur in COVID long haulers. This typically entails a quick heartbeat, when the person switches from a lying position to an upright position. This can also be accompanied by dizziness, drowsiness, and nausea among other things.
2. Lung and respiratory problems (pulmonary symptoms)
Many COVID long haulers have symptoms affecting the lungs. Such symptoms can be, for example, persistent coughing or breathlessness. Breathlessness can occur in resting phases as well as under mild strain, for example, while climbing stairs. Long haulers then frequently have an oppressive feeling in the chest and can no longer take a deep breath.
The pulmonary function diagnosis can provide indications of how heavily the lung is actually affected. It tests, among other things, how much air can the lung take in per breath (respiratory volume). The speed at which the breath flows can also be measured. In people with Long COVID, the lung often has a lower capacity to take up gases and transport oxygen in the blood. In many cases, there are also changes in the lung, which can be seen by X-ray or a computer tomography (CT). Thus, large scars can be found on the lung in many of the patients with the corresponding symptoms. In some long haulers, the blood circulation of the lung has also changed. Of course, the corresponding changes cannot always be found in the examinations.
An increased risk of lung problems was observed in people with asthma. A section of COVID long haulers also has malfunctions in the respiratory muscles.
3. Cardiovascular symptoms
Apart from the lungs, the heart and the circulatory system can also be affected due to a COVID-19 illness. People with high blood pressure or a pre-existing heart condition can be especially vulnerable. Long haulers can suffer from chest pains, a fast heartbeat, skipped heartbeat or a reduced pumping function of the heart.
Various causes are discussed with regard to heart problems. One theory says that the Corona virus reaches the heart muscle and remains there even after an acute illness. A persistent inflammation and reactions of the immune system could then lead to changes in the heart muscle.
The blood vessels can also be damaged. According to some research findings, this can be caused by inflammations and tiny blood clots. Increased frequency of thromboses was also described, for example venous thromboses in the legs. In thromboses, blood forms clots in the vessels and blocks them fully or partially.
4. Problems of brain and nerves (cognitive and neurological symptoms)
Typical Long COVID symptoms also affect the mental capacities as well as the nervous system. According to review, around 22 per cent of the long haulers still suffer from impaired mental abilities 12 weeks after the Corona virus infection. Among other things, long haulers report headaches as well as problems in sensations, memory, or concentration. These symptoms are also called “brain fog” that is, a “hazy feeling in the brain”. Some long haulers find it difficult to speak fluently. They also have the feeling that their brain processes the information slower than prior to the infection. An increased sensitivity to light or noises, dizziness, tinnitus, and loss of hearing have also been described until now.
Researchers analysed 2 years of data of more than one million people after a COVID-19 illness. In the process, they also came to the conclusion that problems of the nervous symptoms can arise as long-term effects. They also found indications of long-term psychological effects. There were 14 different neurological and psychiatric diagnoses in the analysis, which set in after an infection. The most frequent were anxiety and mood disorders, but also dementia, strokes, and psychotic disorders such as schizophrenia. However, we have to bear in mind here that these disorders are anyway prevalent in the population. It is still not verified whether the Corona virus infection was the real cause of these disorders in the long haulers.
It was found in various studies that there were changes in the brain after a COVID-19 illness as a potential mechanism for symptoms. These include, among other things, persistent inflammations in the brain and changes in the blood vessels of the brain with a tendency for blood clots.
5. Type 2 diabetes
A type 2 diabetes could also be a potential long-term effect of COVID-19. A study on this topic from Germany was published in the journal Diabetologia. In the study, type 2 diabetes newly occurred more frequently among 35,000 people after a COVID-19 illness than in a comparison group. This comparison group consisted of people, who had other infectious respiratory disease. Studies from other countries also came to the conclusion that a newly occurring type 2 diabetes can be possible consequence of a Corona virus infection. Meanwhile, there are also studies, which found a link between a Corona virus infection and suffering from type 1 diabetes.
Other damages to organs
Various studies examined the extent to which a Corona virus infection leads to organ damage. Apart from damage to lungs, brain, and heart, damage to the kidneys, liver, pancreas, and spleen have also been found in patients. It is not yet clear how this organ damage develops over time and this needs further research.
Other long-term effects
There are other illness and symptoms that were reported after a Corona virus infection. For example, symptoms that affect the genital organs have been reported. These include menstrual disorders in females such as irregular cycle. Intensified symptoms before regular bleeding also appear to occur more frequently in patients of Long COVID. Erectile dysfunction and infertility have been described as long-term effects in men with Long COVID.
Symptoms related to the digestive system can also occur in the wake of Long COVID. These include stomach ache, nausea, loss of appetite, diarrhoea and constipation. A change in the composition of the intestinal bacteria (gut flora) has been described in COVID long haulers. The extent to which this is connected with various symptoms has not been conclusively explained yet.
Other symptoms and long-term effects such as sleep disturbances or autoimmune diseases have also been described. Which long-term effects should be distinctly attributed to the Corona virus infection is not conclusively clear yet. We also cannot conclusively say yet, how frequently and in which combination the symptoms can arise. Further research is necessary to understand these things in-depth and to be able to help long haulers accordingly.
What is a PICS?
Long haulers, who had to be treated in intensive care units owing to COVID-19 can suffer from a “Post-Intensive-Care-Syndrome” (PICS). A PICS can also occur after other sever illness with treatment in an intensive care unit. Potential symptoms of a PICS are muscle weakness as well as mental and psychological disorders. These impairments can turn out to be serious.
Sources:
https://register.awmf.org/assets/guidelines/020-027l_S1_Long-Post-Covid_2025-08-verlaengert.pdf
https://www.nature.com/articles/s41579-022-00846-2
https://www.mdpi.com/2075-4418/14/7/711
https://www.mdpi.com/2227-9059/12/4/913
https://www.mdpi.com/2077-0383/12/3/1159
https://pmc.ncbi.nlm.nih.gov/articles/PMC10408714/
https://www.annualreviews.org/doi/pdf/10.1146/annurev-med-043021-030635
https://link.springer.com/article/10.1007/s10067-023-06670-0
https://jamanetwork.com/journals/jama/fullarticle/2805461
https://www.pschyrembel.de/Posturales%20orthostatisches%20Tachykardiesyndrom/B07T4
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02656-y
https://www.nature.com/articles/s41598-022-24185-7
https://www.primary-care-diabetes.com/article/S1751-9918(22)00100-0/fulltext
https://link.springer.com/article/10.1007/s00125-022-05670-0
https://www.herzstiftung.de/ihre-herzgesundheit/coronavirus/post-covid-herzschaden-therapie
https://www.sciencedirect.com/science/article/pii/S0889159121006516?via%3Dihub
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
https://www.thelancet.com/journals/landia/article/PIIS2213-8587(22)00044-4/fulltext
https://link.springer.com/article/10.1007/s00108-022-01371-3
Last update: December 2024
What is the prognosis of Long COVID?
The prognosis of Long COVID cannot be conclusively determined yet. This is partly because the results of the studies until now cannot be applied to the entire population. Various studies have various indications that symptoms of Long COVID recede or disappear completely in many long haulers in the first few months. But the symptoms can also persist longer than 12 months.
Researchers investigated the findings of long haulers after their COVID-19 illness over a longer period of time in some studies. 137 studies with a total of 134,093 participants were evaluated in a comprehensive review. While around 92 per cent of the patients still had symptoms directly after a COVID-19 illness, the number was only 55 per cent after a month. After one year, only around 50 per cent of the long haulers reported of still having symptoms. There also appear to be variations in individual symptoms. Thus, this review as well as other studies suggest that symptoms relating to the nervous system and psyche persist longer than other symptoms. Such symptoms as follows were still reported after 12 months: Sleep disorders (30 per cent), problems in concentration (27 per cent), depression (26 per cent), anxiety disorders (25 per cent), post-traumatic stress disorder (23 per cent) and problems with memory (19 per cent). 12 months after their COVID-19 illness, the COVID long haulers still reported the following physical symptoms: Shortness of breath (21 per cent), exhaustion and muscle weakness (20 per cent), breathlessness (14 per cent), tightness in the chest (13 per cent), joint ache (11 per cent) and hair loss (11 per cent).
It was found in various studies that Long COVID occurred more frequently in patients if they had to be treated in the hospital. The symptoms also appeared to last longer in these people. However, the results until now are not uniform in this regard and further long-term research is necessary.
Studies on the course of Long COVID in children show that most of the children recover with time. But in a small number of cases, the symptoms appear to persist longer. Apart from that, there are indications of Long COVID symptoms receding faster after an infection by the Omicron variant than after and infection with earlier variants.
In summary, the study results until now indicate that the course of Long COVID varies greatly from person to person. In particular, some symptoms appeared to decrease or completely disappear in the first few months. If the symptoms still persist then, they can sometimes also last for a longer-term. This is especially true for symptoms affecting the psyche and nervous system. But overall, further long-term research is still needed to gain reliable data.
Sources:
https://www.valueinhealthjournal.com/article/S1098-3015(22)04743-X/fulltext
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00138-4/fulltext
https://www.nature.com/articles/s41380-022-01614-7
https://www.sciencedirect.com/science/article/pii/S2666991922000380?via%3Dihub
https://jamanetwork.com/journals/jama/fullarticle/2797443
Further information:
Last update: December 2024
Do Long COVID and ME/CFS overlap?
What is ME/CFS?
ME/CFS is the abbreviation for Myalgic Encephalomyelitis or Chronic Fatigue Syndrome. The ME/CFS illness is a severe and persistent illness affecting various bodily systems. It affects, among others, the nervous and immune systems. It frequently begins after viral diseases. Women are affected more often than men. A severe exhaustion (also called “fatigue”) that lasts for several months and impairs daily life is typical of ME/CFS. The leading symptom in ME/CFS is also a so-called stress intolerance, also known as PEM (Post Exertional Malaise). In stress intolerance, the symptoms can aggravate already after light everyday exertions such as a meeting or a household activity (so-called “crash”). The worsening mostly sets in only after several hours or on the next day. It often lasts for several days, weeks or even longer. Besides fatigue and stress intolerance, other physical and mental symptoms of different severities can also arise in ME/CFS. These include muscle aches, headaches, and aching limbs, a disturbed sleep and problems in concentration. The diagnosis of ME/CFS is made by means of certain diagnostic criteria. These criteria relate to the symptoms and their course. Until now, there is no appropriate lab value that can be used to reliably diagnose ME/CFS. ME/CFS can greatly affect the quality of life. Many long haulers are incapable of working. In extremely severe cases, the patients are bed-ridden and in need of care.
Based on an order of the Federal Ministry of Health, the institute for quality and efficiency of healthcare (IQWiG) examined the current scientific insights on ME/CFS and summarised them in a report. The essential points of the report deal with the current state of knowledge on ME/CFS, especially on aetiology, symptoms, risk factors, prevalence, course of illness, diagnosis, and rehabilitation as well as evidence charging and usage evaluation of the relevant therapy options.
Apart from that, a so-called Consensus statement for diagnosis and treatment of ME/CFS was published in May 2024. This publication summarises the current state of knowledge on ME/CFS including the diagnosis and current treatment options.
You can read more about this under the question “What are the scientific insights until now for treatment of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS)?”.
What is the connection between Long COVID and ME/CFS?
Viral diseases are a frequent cause for ME/CFS, for example, after an influenza virus or Epstein Barr Virus (EBV) infection. ME/CFS can occur even after a Corona virus SARS-CoV-2 infection. According to the reports of the National Association of Statutory Health Insurance (KBV), initial data from health insurance companies also confirm the hypothesis that ME/CFS was detected more frequently as a consequence of COVID-19 pandemic.
There is a series of possible underlying mechanisms discussed for Long COVID as well as for ME/CFS. These include changes in the area of nervous system, immune system, and the performance of the cardiovascular system.
No definitive statement on the frequency of ME/CFS after a Corona virus infection can be made based on the data until now. Extensive studies are necessary for substantiated findings. In addition, in-depth research on the causes of Long COVID and ME/CFS is necessary.
Further details of the current research projects and their funding can be read under the question “How are the Federal Ministry of Health (BMG) and Federal Ministry of Education and Research (BMBF) promoting research on Long COVID and ME/CFS?”.
Sources:
https://link.springer.com/article/10.1007/s00508-024-02372-y
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1090747/full
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00323-1/fulltext
https://lost-voices-stiftung.org/zusammenhang-zwischen-long-covid-und-me-cfs/
https://www.iqwig.de/download/n21-01_me-cfs-aktueller-kenntnisstand_abschlussbericht_v1-0.pdf
Further Information:
https://www.iqwig.de/projekte/n21-01.html
https://www.rki.de/DE/Content/GesundAZ/M/ME_CFS/ME_CFS_inhalt.html
https://www.thieme-connect.de/products/ejournals/abstract/10.1055/a-1849-8953
Last update: December 2024
What other support services are in place?
With the help of the Doctor search of the National Association of Statutory Health Insurance Physicians (KBV) you can find doctors of all specialities in your area. The search is also available in the app “116117.app”.Some health insurance companies offer their members advice or online services on corona virus, COVID-19 and Long COVID.
In addition to doctors' surgeries, health insurance companies and specialised outpatient clinics for Long COVID, there are many other places where those affected or their relatives can find help:
Psychotherapeutic support
It may be advisable to seek psychotherapeutic support if you are under emotional stress. The family doctor’s practice is also the first port of call for this. Long haulers can search for psychotherapy clinics in their surroundings on the website of the German Psychotherapy Association.
In the case of Long COVID, so-called benefits for participation may also be considered. Such benefits are intended to help people lead a self-determined life. This can include, for example, support in coping with everyday life independently, in leisure activities or in living, such as housekeeping. Free information on this topic is provided, for example, by the Supplementary independent participation counselling (EUTB®). Here, those affected can obtain advice on the possibilities for support in their personal situation.
Self-help groups and initiatives for affected persons
As with many other diseases, it can be helpful and beneficial for people affected by Long COVID and their relatives to share their experiences. The National Contact and Information Centre for the Initiation and Support of Self-Help Groups (NAKOS) provides an overview of offers for self-help and self-help groups. A leaflet of NAKOS can serve as an initial orientation guide. You can also take a look at the Long COVID platform operated by the BAG Selbsthilfe (German Self-Help Association) for an overview of various self-help groups throughout Germany. Self-help groups exist in various formats, both digital and face-to-face.
In addition to self-help groups, there are also initiatives for those affected. These were founded by affected persons with great commitment and they serve to support each other and to provide offers of help as well as information. The “Long COVID Deutschland” initiative has been created from an online self-help group on Facebook. The website now provides information for affected persons and relatives on many topics relating to the pathology.
Health apps
Nowadays, there are also apps for people affected by Long COVID, which are offered by several health insurance companies in Germany. Apps can accompany people in their daily lives and help them cope with the disease.
Insured persons can ask their health insurance company whether an app is already offered as a health insurance benefit. If it is not yet the case, you can submit an application for cost coverage.
Telephone counselling
Our citizens’ hotline provides information on counselling and support services for Long COVID in Germany, specifically tailored to your region. Individual states also offer a phone consultation programme for COVID long haulers and people with Post-VAC. For example, there is such a programme in North Rhine-Westphalia and Lower Saxony.
Long COVID in a professional context
Please also note our information specifically for employees and employers. In the section "Things to know about Long COVID in the occupational context" you will find information and contact points on topics such as Long COVID as an occupational accident, occupational absences due to Long COVID, Long COVID in daily working life and resuming work.
Further information and support services
You can take a look at an overview of further information and support services on our website in the service area.
Sources:
https://www.gesundheitsinformation.de/wege-zur-psychotherapie-wo-gibt-es-hilfe.html
https://www.teilhabeberatung.de/beratung/beratungsangebote-der-eutb
https://www.nakos.de/themen/corona/
https://www.nakos.de/data/Materialien/2022/NAKOS-Faltblatt-Hilfe-nach-Covid-19.pdf
Last update: December 2024
Dealing with Long COVID
What can you do to protect yourself against Long COVID?
The best-possible protection against Long COVID according to the current state of knowledge is avoiding a Corona virus SARS-CoV-2 infection as much as possible. This is also true for a repeat infection.
It can also be hypothesised from the research results until now that the Corona vaccination also protects from Long COVID to a certain extent. The Corona vaccination protects against a severe course of a COVID-19 illness. Patients with a severe COVID-19 illness in turn have a higher risk of Long COVID. Furthermore, there are indications that a complete Corona vaccination can reduce the frequency and severity of Long COVID symptoms. In a review conducted in 2023, the results from multiple studies with a total of over 500,000 participants were evaluated. According to it, people who were vaccinated twice were at a lower risk of Long COVID as compared to the people vaccinated once or those who were not vaccinated at all.
The following behavioural measures can help in lowering the risk of Corona virus infection as much as possible.
- In times with many respiratory infections, wearing a mask indoors can make sense, especially if there are many people there and sufficient distancing is not possible.
- Regular intermittent full ventilation of indoor spaces is useful.
- If you have respiratory illness, you should stay at home as far as possible and limit contact with other people. Wearing a mask is useful for unavoidable meetings with other people.
- Washing your hands properly is important. It also reduces the risk of getting other pathogenic infections.
- Apart from that, you should follow the rules of hygiene while coughing and sneezing (for example, sneeze in the crook of the arm)
You can get more information on possible protection measures against Corona virus at the Federal Centre for Health Education (BZgA). There, you will also find information on Corona vaccination for children, adolescents, adults and pregnant women. You can receive your current vaccination recommendation with the help of Corona vaccination-check.
Sources:
https://www.sciencedirect.com/science/article/pii/S0264410X23001342?via%3Dihub
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2802877
https://bmjmedicine.bmj.com/content/2/1/e000385
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00354-6/fulltext
https://www.impfen-info.de/impfempfehlungen/
https://www.infektionsschutz.de/coronavirus/fragen-und-antworten/sich-und-andere-schuetzen/
Further information:
https://www.infektionsschutz.de/coronavirus/schutzimpfung/der-corona-impfcheck/
https://www.rki.de/DE/Content/Kommissionen/STIKO/Empfehlungen/Impfempfehlungen_node.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9261894/pdf/108_2022_Article_1368.pdf
Last update: December 2024
What are the first steps in case of a suspicion of Long COVID?
If you suspect that you are afflicted with Long COVID, you should initially contact the family doctor. The paediatric practice is the first point of contact for children and adolescents. The first clarification will take place in the family doctor’s or paediatric clinic. This includes a detailed inquiry of the symptoms, their course and accompanying conditions as well as a comprehensive physical examination.
According to the so-called Long COVID Guideline of Joint Federal Committee (G-BA), the family doctor or paediatrician serves as the central contact person for the long haulers and coordinates the further treatment. The guideline came into force in May 2024 and describes the care and treatment paths if there is a suspicion of Long COVID, ME/CFS or similar illnesses after an infection.
If needed, the attending doctor can also assign another specialist’s clinic and mediate an appointment there if applicable. The latter can be especially sensible in urgent cases. In the meanwhile, there are various COVID-19 specialised practices as well as special consultation hours for COVID long haulers. The visit to a special outpatient clinic especially makes sense when the symptoms last longer or deteriorate. Even in case of a suspicion of stress intolerance with deterioration of the symptoms (“Post Exertional Malaise” abbreviated PEM), or suspicion of ME/CFS, it is useful to visit a specialist doctor. You can also find specialised points of contact using our community helpline. Also read the answer to the question “Where can I find appropriate competence centres or special outpatient clinics for COVID long haulers?”
You should bring along your personal medical documents for all the appointments, if such documents are available. These include, for example, medical findings or medication regimes. The doctors can then match the treatment precisely to the needs of the sick person.
Important: There are no certain “Tests” or lab investigations yet, which can unambiguously prove Long COVID. Instead of it, other reasons for the symptoms must first be ruled out. So, for example, the cause of tiredness or problems in concentration can also be other illnesses, deficiencies, stress or strenuous life situations.
Further information on possible examinations for typical complaints can be found in the patient guideline ‘Long/Post COVID syndrome’. You can also find more detailed information in the ‘Guideline for healthcare professionals’.
Help in searching for a hospital, a doctor’s practice or outpatient clinic:
https://dkgev.deutsches-krankenhaus-verzeichnis.de/app/suche
Last update: August 2024
What can long haulers themselves do in case of Long COVID symptoms?
In a Long COVID illness, the long haulers should follow the treatment, which has been coordinated with the doctor. In addition, patients themselves can do a few things to improve their own health or to find a good way to deal with the symptoms.
A balanced lifestyle can have a positive effect on physical and mental health. This means: It is important to look after yourself and not to neglect your own needs. This can also mean a walk in the fresh air or taking a break on the sofa. Alcohol and smoking should be avoided if possible. Eating a balanced diet and keeping yourself hydrated enough also supports your own health. In the patient guideline ‘Long/Post COVID syndrome’ you will find precise nutritional recommendations and other measures you can take to promote your health. Good to know: With a balanced diet, it is generally not necessary to take dietary supplements such as vitamin supplements.
Good to know: If you suspect a vitamin or micronutrient deficiency, you should not take supplements such as vitamin products “on suspicion”. The potential deficiency should first be medically clarified and then specifically treated.
Persons affected by Long COVID can find it difficult to talk about their symptoms with those around them. However, being open about the illness often helps to get support. Friends and family can help with everyday life or support in organising medical appointments. They can also support those affected during visits to the doctor. Sometimes it is also helpful to talk to other affected persons or relatives.
Note:
For all the techniques for dealing with Long COVID symptoms: As the illness is extremely varied, it also applies that different things help different people. The exercises and strategies listed below should not be the sole treatment but always supplement the medical treatment. In addition, long haulers should coordinate these measures with the attending doctor.
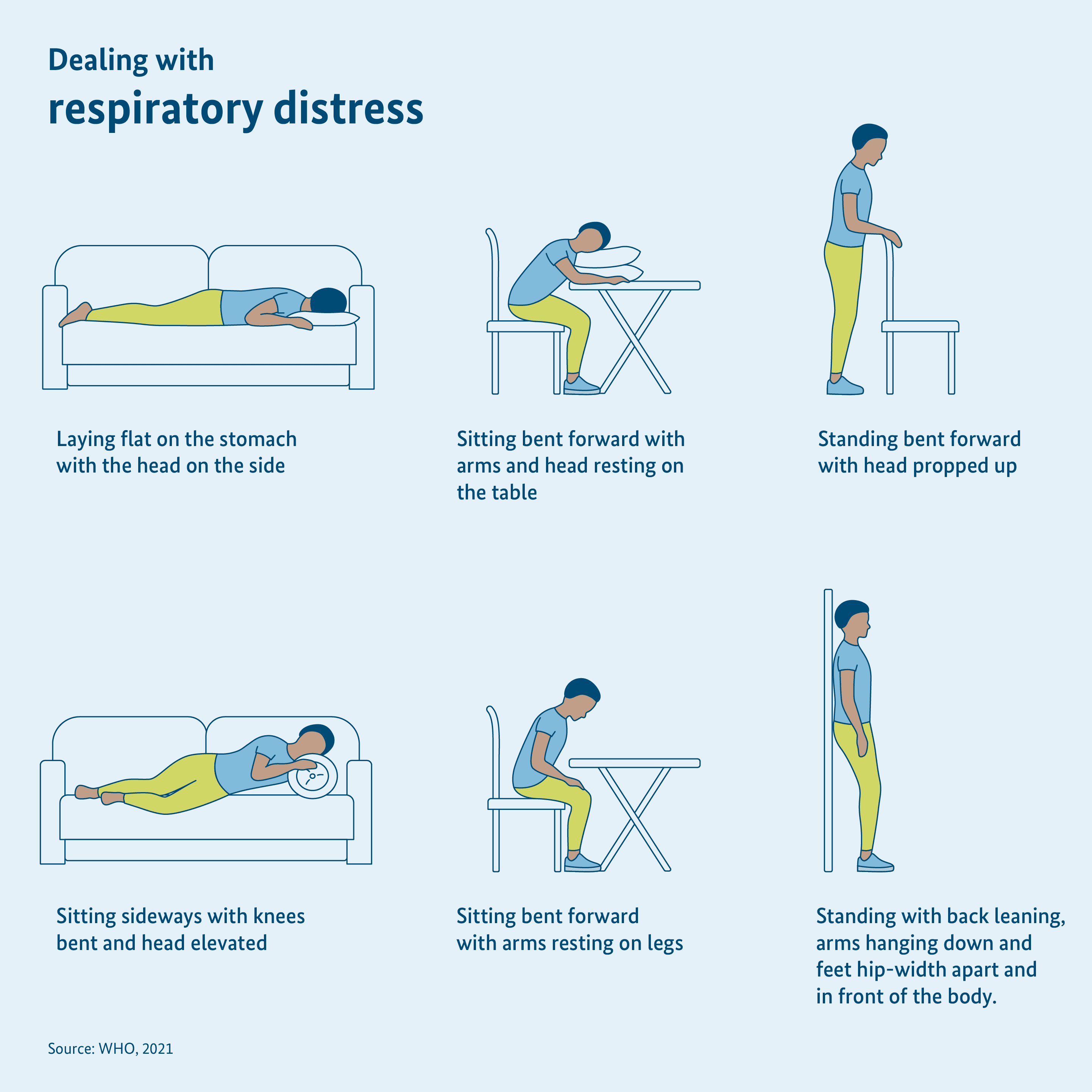
1. Handling breathlessness
Pressure on the chest, shortness of breath or the feeling of not getting enough air can cause anxiety. It is important to stay calm in order to not reinforce such feelings. If you feel overstrained after brief exertion and you start getting breathless, a break can help. Then the breathing can normalise.
You can also take up various body postures that make breathing easy. These include:
- sitting leaning forward with arms laid down on the table and head laid down
- flat prone position with the head turned to the side
- lying on your side with bent knees and elevated head
- sitting leaning forward with arms laid down on the legs
- standing leaning forward, with support
- standing with the back leaning on the wall, drooping arms and feet hip-width apart
Long haulers can also learn certain breathing techniques such as even and controlled breathing. It can help to get air better in light everyday activities.
2. Exercise and sporting activity
If long haulers had to spend a long time at home or in the hospital because of contracting COVID-19, then the muscles can become weak. The physical capacity is probably greatly restricted. That is why, exercise is important to gradually recover the strength and endurance. Movement can also have a positive impact on symptoms of Long COVID. It is therefore helpful for some long haulers to integrate various physical activities in their daily routine. But while doing so, you must strictly pay attention to your own body. If you suffer from quick exhaustion (fatigue) or a stress intolerance, a brief exertion can already worsen the symptoms. In this case, long haulers should organise their own resources as sparingly as possible and avoid strains, which can lead to a worsening. More information on this strategy called pacing is given in our answer to the question “What is pacing?” and the website of the German Society for ME/CFS.
As long as there is no stress intolerance, there are various options for more activity. For example, you can try to move for at least a total of 30 minutes a day. Movement includes among other things walking, cycling, climbing the stairs, or even gardening. Depending on your own capacity, the activities can be gradually increased with time. The so-called Borg-scale can be helpful to this end. Here, the long haulers estimate various activities and state how strenuous they feel these on a scale of 0 to 10. 0 is the resting state or rather no exertion, and 10 the value for maximum exertion. Maintaining a stress diary can help. Long haulers can grade all the activities that they do in everyday life in the diary. In this way, you can learn to listen to your body. In addition, you can gradually step up the strains as you feel. While doing so, you should check regularly whether the extent of sports activities is good for you and if some of the symptoms are improving by this activity.
Even simple exercises that you can do at home without aids are helpful. Examples of such strengthening exercises can be found in the WHO brochure ‘Recommendations to support independent rehabilitation after COVID-19-related illness’ from page 11.
Sources:
https://apps.who.int/iris/handle/10665/340306
https://apps.who.int/iris/bitstream/handle/10665/345019/WHO-EURO-2021-855-40590-60116-ger.pdf (p. 8)
https://register.awmf.org/de/leitlinien/detail/020-027
Further Information:
https://register.awmf.org/de/leitlinien/detail/020-027
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2817149
3. Dealing with persistent exhaustion
Many COVID long haulers report tiredness and physical and mental exhaustion, which frequently recurs or continues. In any case, long haulers should first talk to their doctor as these symptoms are not of just ordinary exhaustion. A so-called “stress intolerance” also occurs in some COVID long haulers. Their symptoms can already aggravate after mild physical or mental exertion. Pacing has proved to be successful in stress intolerance. Pacing is a strategy to properly handle your own strengths.
According to this strategy, long haulers should try to design everyday life according to the available strengths. Setting your priorities and planning properly in advance is important. Wherever possible, initially you can put aside tasks that are not absolutely necessary. It is also helpful if many strenuous activities are not done one after the other. Perhaps you can do one or the other task at another time or request others for assistance.
In addition, it is important to regularly make room for breaks and recovery. A diary or notebook can help in maintaining an overview.
The most important thing is to listen to your body and to look after yourself with care. You have to treat yourself like a person, who is close to your heart. People are often much harder on themselves than on those, who are the closest to them. Your own health should be your first priority. You can find out more about how to manage your own strength appropriately under ‘What is pacing?’.
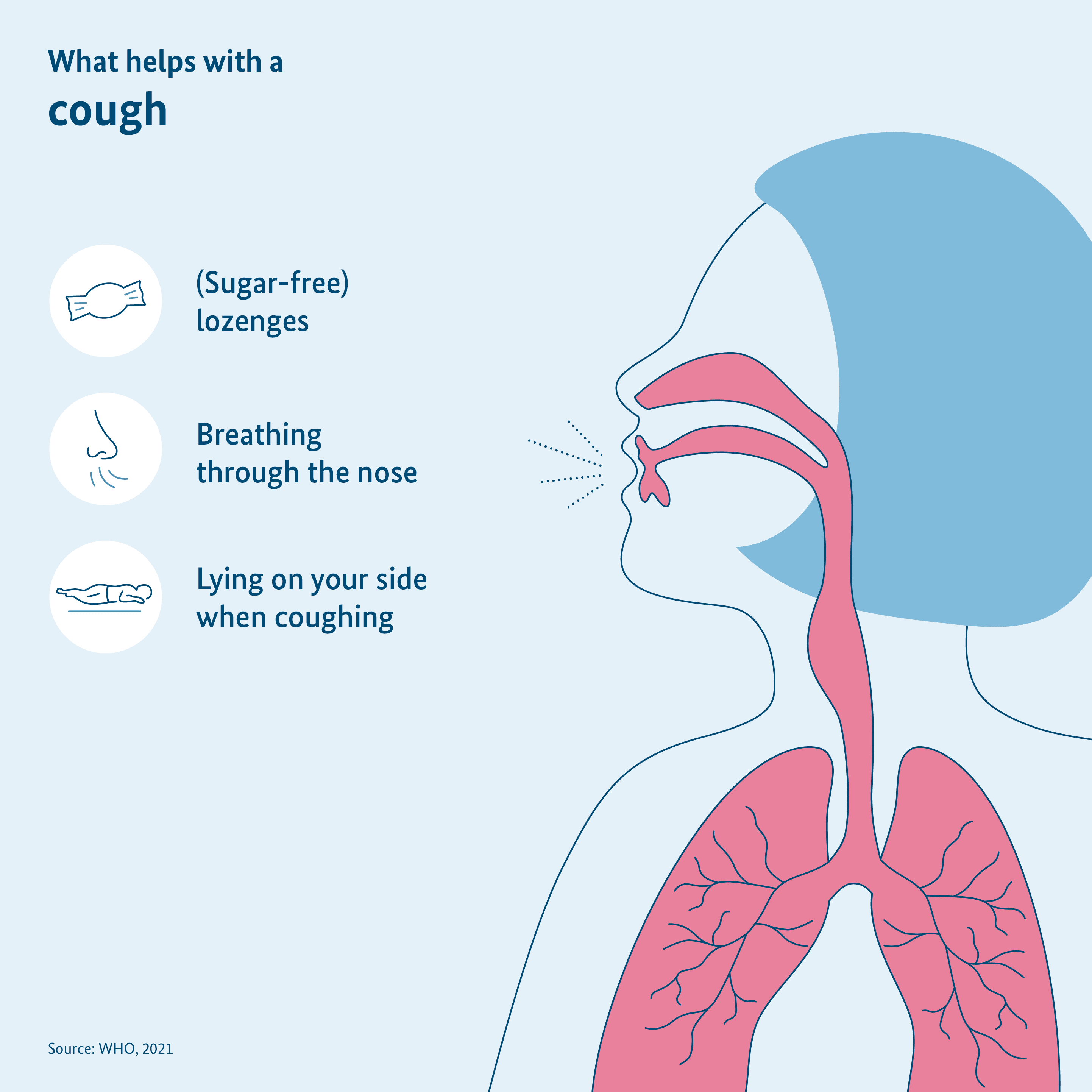
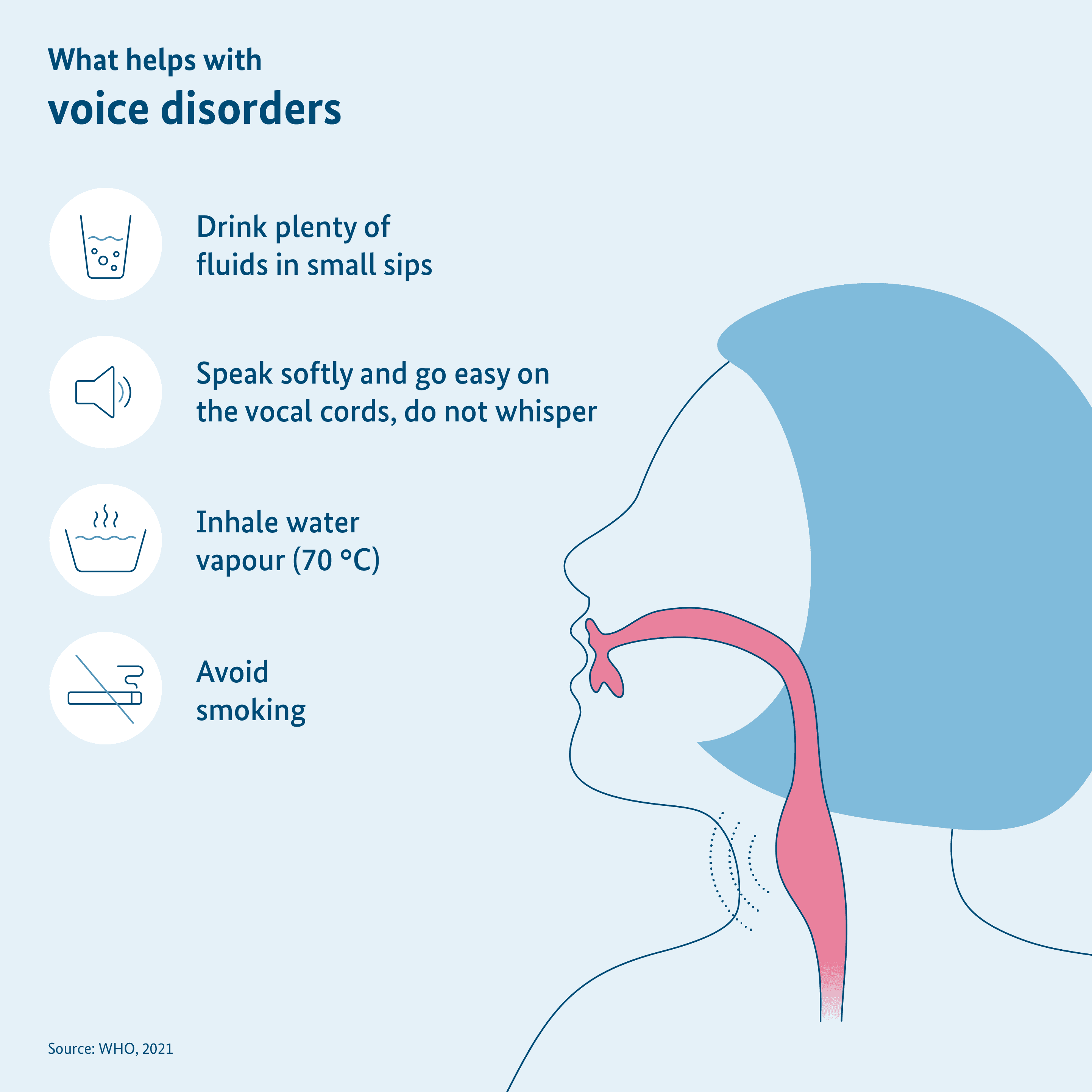
4. Dealing with cough and voice disorders
Cough and voice disorders occur frequently after a COVID-19 illness. Many patients report a constant scratching in the throat, which makes them cough. They get hoarseness or their upper respiratory tract and vocal chords are filled. Then there are some things that the long haulers can do:
- Long haulers should drink a lot of fluids throughout the day so that the throat does not become too dry.
- The voice should be rested and hence you should speak softly, but not whisper. Whispering greatly strains the vocal chords.
- You can inhale steam to moisten the vocal chords and alleviate the irritation in the throat. Inhalers are available in the pharmacy. In the old household tradition, you can also inhale steam from hot water in a bowl. But the water must not be boiling! Be careful of not scalding yourself.
- Avoid smoking because it aggravates the symptoms.
- Boiled sweets can moisten the throat. They should be sugar-free as far as possible. There are also special sweets in the pharmacy, which can alleviate the hoarseness.
- Breathing more through your nose than you mouth can help. That warms up the air before it reaches the lungs and hence reduces the feeling of irritation.
- Long haulers often have to cough lying down. It can help in these cases to lie on the side or elevate the head with some pillows.
- In case of severe irritation of the throat, you can also perform specific exercises that reduce the irritation.
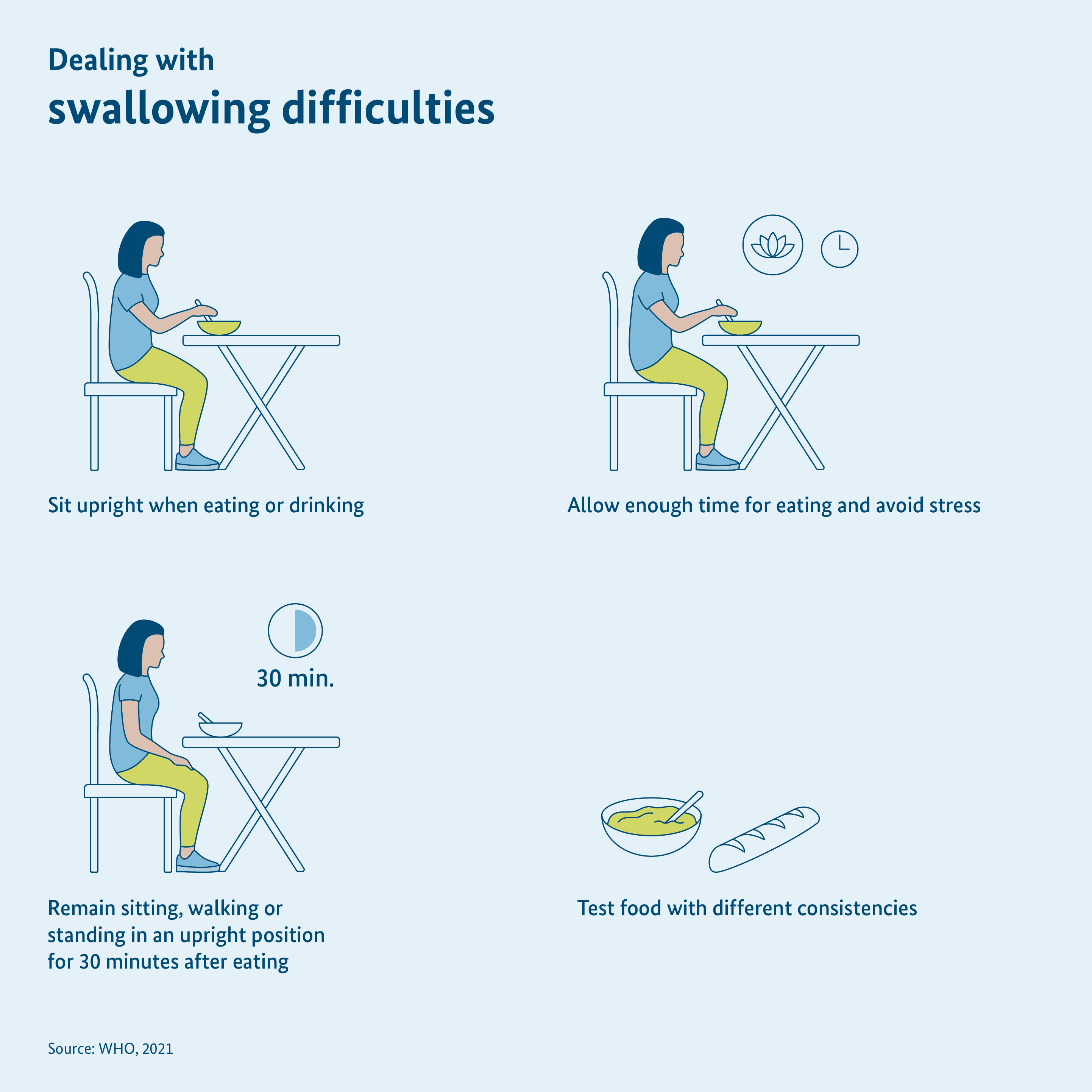
5. Dealing with difficulty in swallowing
If swallowing foods or beverages is difficult, then long haulers should sit up and under no circumstances take meals while lying down. As far as possible, you should spend a few more minutes in upright posture, so sitting, standing or walking. Meals with different consistencies can also be tested. Porridges or soups are often easier to swallow than “sharp foodstuffs” such as baked baguette.
While eating, you should also avoid stress and plan in enough time. Thorough chewing also helps in ensuring that too big portions do not have to be swallowed. Overall, attentive eating and drinking will also assist.
6. Dealing with impaired sense of smell and taste
If long haulers cannot smell or taste well or not at all, good oral hygiene is especially important. The teeth should be brushed twice a day and regularly cleaned with floss. However, it is also possible to stimulate the olfactory nerves and taste buds in different ways. For example, you can carry out a specific smell training. For this exercise, you can smell smell-intensive plants and spices such as clove, lemon, cinnamon, peppermint, or eucalyptus, for 20 seconds multiple times a day. You can also experiment with new spices or fresh herbs while cooking. But be cautious while doing so. Herbs and spices can aggravate the symptoms if you suffer from heartburn.
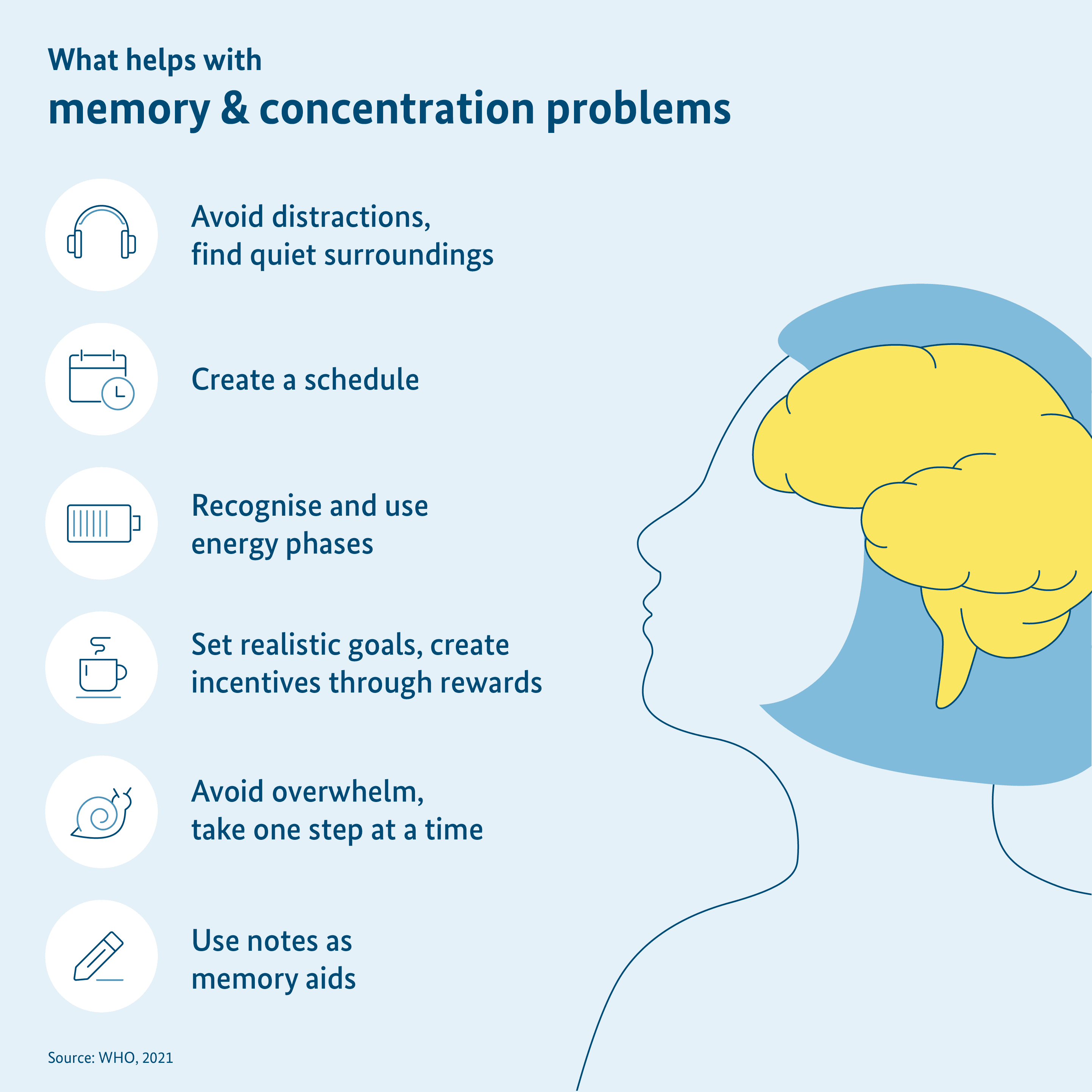
7. Dealing with problems with memory or concentration
Problems with concentration and memory rank among the symptoms in Long COVID most frequently voiced by long haulers. In such cases the following notes are helpful:
- If long haulers pursue mentally challenging tasks, they should avoid distraction while doing the task. A peaceful environment with less outside noise or environmental stimuli as well as earplugs can be of help here to reduce the noise level.
- A time plan with realistic goals also helps. Long haulers should overexert themselves and approach the tasks step by step.
- Regular breaks are indispensable.
- It is best to pursue activities when you feel rested and relaxed. It can vary from person to person: While there are those who are the most focussed in the morning and get tired over the course of the day, there are others, who work in the evenings.
- Perhaps, incentives can help here in feeling motivated. They can be small things such as a cup of coffee or a walk in outdoors.
- Long haulers should pace themselves. Many people have the feeling of needing to “accomplish” something. They feel guilty if their goal is not achieved. But this frustration can lead to them feeling blocked and then being able to concentrate lesser. Even though it is easier said than done: It is important to deal with yourself carefully and not overexert yourself with too much work.
- Memos or notes in the Smartphone or calendar can help in memory problems.
8. Dealing with states of anxiety, depressions, and sleep disturbances
If long haulers have extraordinarily severe anxiety, panic attacks or a depression, they should contact their doctor. The doctor can help in receiving therapeutic support if necessary. But even here, you can take measures to improve your own well-being.
- As far as possible, long haulers should surround themselves with people who will do them good. Even if depressive resentments are often accompanied by the desire for retreat, social contacts are beneficial. Loneliness can worsen the problems. Social contacts, on the other hand, help to reduce stress and get support.
- Similarly, pursuing a hobby or taking up a new hobby can also help.
- Activities such as yoga, meditation, relaxing baths or listening to music can also probably help in relaxing you.
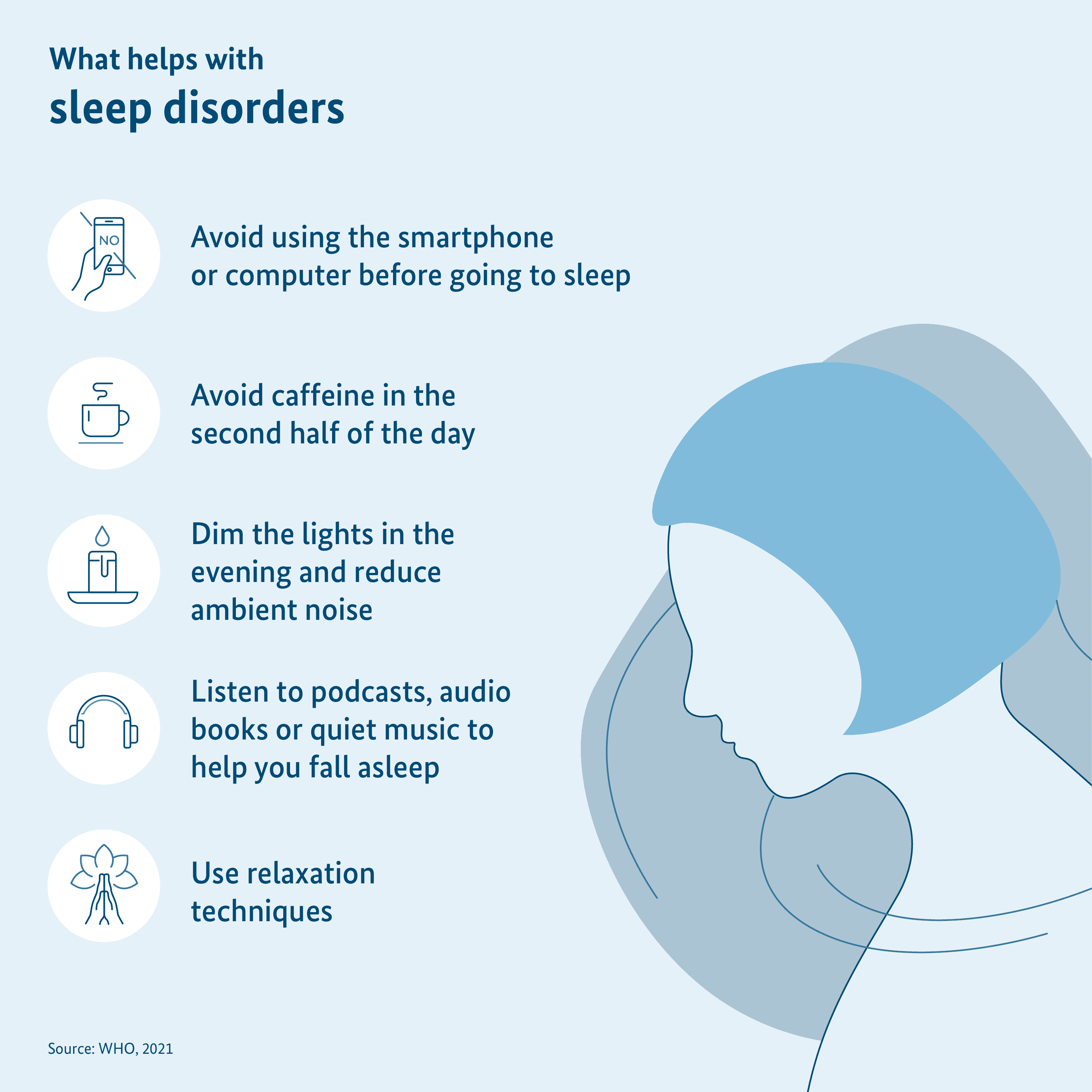
- A healthy sleep is especially important for the general well-being. Some techniques can be helpful while falling asleep:
- If the eyes perceive a lot of impressions, it can be stimulating for the brain. That is why it can be helpful to not spend time on the looking at the Smartphone or computer screen 1 to 2 hours before falling asleep.
- In the second half of the day, you should avoid stimulating ingredients such as nicotine or caffeine as much as possible. Caffeine is in for example, coffee, energy drinks and black and green tea.
- It can help some people to dim the light in the evening and reduce the surrounding noises.
- Calming music, podcasts or audiobooks can also assist in falling asleep.
- Focussed relaxation techniques can also be used.
Last update: December 2024
What is pacing?
Pacing is a strategy to deal with fatigue or stress intolerance (an explanation of these symptoms is given in the answer to the question “Which symptoms can arise in Long COVID?”). It is frequently recommended for COVID long haulers and has already been use for a long time for Myalgic Encephalomyelitis or Chronic Fatigue Syndrome (ME/CFS). Pacing is handling your own strengths sparingly. In this, the long haulers should learn to carefully listen to their own body and organise their strengths properly. This includes, for example, recognising and adhering to your own stress limits.
The goal of pacing is that the so-called “Crashes” occur more infrequently and have a less severe progression. In a “Crash”, the symptoms already aggravate after mild physical or mental exertion.
Pacing should support long haulers in organising their activities and energy reserves. A diary can help to observe their own behaviour and to be able to better estimate the consequences over time. Thus, long haulers can proactively plan their activities including regular breaks. It can also be helpful to incorporate specific relaxation exercises. Among other things, a step count can be useful for affected persons to measure as to with how much exercise they feel well or bad. Then they can determine the limit for exercise. In addition, there are other methods to avoid overexertion. For example, long haulers can measure their heartbeats at rest and under stress. The use of mobile apps or fitness wristbands for this purpose can be helpful.
Important to know: In contrast to activating approaches, the aim in pacing is not to increase the activities gradually. According to the current state of knowledge, an activating therapy, where your own stress limits are not taken into account, can deteriorate the condition of the long haulers.
You will also find an explanation on how exactly pacing works on the information site of the Deutsche Gesellschaft für ME/CFS e. V. It also has a corresponding Guideline.
Pacing plays an important role in the daily life of ME/CFS patients and is recommended by various ME/CFS research networks across Europe. However, further research is still necessary to gain in-depth insights in the advantages and disadvantages of this strategy.
Sources:
https://www.mecfs.de/was-ist-me-cfs/pacing/
https://link.springer.com/article/10.1007/s00508-024-02372-y
https://register.awmf.org/de/leitlinien/detail/020-027
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10722442/
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1247698/full
Further information:
https://www.mecfs.de/wp-content/uploads/2022/04/DGMECFS_Pacing_A4.pdf
https://www.omf.ngo/wp-content/uploads/2019/09/PEM-Avoidance-Toolkit-Deutsch.pdf
Last update: December 2024
What are the scientific insights until now for treatment of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS)?
The current state of knowledge for treatment of ME/CFS is limited. Little is understood yet about the illness and there are still no high-quality scientific studies on its treatment. So far, the management of individual activities and energy (“pacing”) as well as the targeted, alleviating treatment of individual symptoms has come to the fore.
ME/CFS is typically accompanied by a stress intolerance. Depending on how pronounced the stress intolerance is, the symptoms can already aggravate after usual everyday stresses. This aggravation can last for hours, or even many days and weeks (so-called “crash”). If you constantly overstrain yourself, there can be long-term or even permanent deterioration. It is therefore important to align any activities to your stress limits during treatment. This “pacing” shall avoid your condition from deteriorating. The approach was developed as a part of the ME/CFS research and is also recommended by the pan-Europe ME/CFS research network EUROMENE.
The institute for quality and efficiency of healthcare (IQWiG) examined the current scientific insights on ME/CFS and published it in May 2023. The conclusion was that an activity therapy does not offer any evident benefit. Long haulers as well as researchers have reported that the symptoms can possibly seriously worsen by activity therapy.
IQWiG had also investigated whether a cognitive behavioural therapy can benefit ME/CFS patients in any way. The evaluation turned out to be positive here. The cognitive behavioural therapy is a form of psychotherapy, where a person, for instance, works on their own thoughts and expectations as well as behaviour. For example, the report says that this treatment can have short-term and mid-term positive effects on fatigue, social participation or malaise after exertion. This is especially true for mildly affected patients.
Important to know: Psychotherapy is supportive in ME/CFS: Now, the patients severely affected by ME/CFS are massively hampered due to the illness and sometimes stressed by social consequences. The aim of a psychotherapeutic support though is not to heal the ME/CFS. Individual stress limits should also be respected in psychotherapy. Trained psychotherapists can also help in the process of learning pacing techniques.
Apart from that, the alleviating treatment of the individual symptoms is important in the ME/CFS therapy. There are initial indications from scientific studies as to which treatments could be helpful. However, we will still need further research for reliable insights. It is sensible that long haulers with ME/CFS and similar Long COVID symptoms discuss with their doctors as to which treatments are worth considering for the patient.
You can find further information in the so-called Consensus statement for diagnosis and treatment of ME/CFS and in an Article of the Deutsches Ärzteblatt [German medical journal] for diagnosis and therapy of ME/CFS. The page of Charité Fatigue Centre also offers information on the current state of knowledge.
Last update: December 2024
Where can people with Long COVID find appropriate centres of expertise or specialised outpatient clinics?
By now, there are various points of contact for people with Long COVID symptoms, whom they can address themselves to. However, the number of requests for help is indeed overwhelming. Therefore, the search for a suitable outpatient clinic can take a long time.
The initial consultation should be at the office of your primary care physician. This office will coordinate further assessments with specialists, as well as supportive treatments such as physiotherapy, respiratory therapy, occupational therapy, or rehabilitation.
The visit to a Long COVID special outpatient clinic or a competence centre should be coordinated with the family doctor. Family doctors are mostly familiar with special outpatient clinics and special clinics in the region and can provide precise help.
With the help of the Doctor search of the National Association of Statutory Health Insurance Physicians (KBV) you can find doctors of all specialities in your area. The search is also available in the app “116117.app”. Affected people can also check the website of their health insurance company. Most health insurance companies now offer guidance to help with the search.
The German Hospital Directory also offers a special search function. In this, people affected can filter the search results specifically according to their region and the keywords "Long COVID" or "Post COVID". This allows them to find suitable hospitals.
Our citizens’ hotline provides information on counselling and support services for Long COVID in Germany, specifically tailored to your region. Individual states also offer a phone consultation programme for COVID long haulers and people with Post-VAC. For example, there is such a programme in North Rhine-Westphalia and Lower Saxony.
You can also find a list of medical practices, clinics and outpatient clinics in Germany on our website in the service area, so that people affected by Long COVID can get in touch with them.
Last update: November 2024
How are the Federal Ministry of Health (BMG) and Federal Ministry of Education and Research (BMBF) promoting research on Long COVID and ME/CFS?
The Federal Government considers it extremely important to support scientists in basic research, clinical research and healthcare research. The Federal Ministry of Health (BMG) initiates projects within the framework of departmental research. The Federal Ministry of Education and Research (BMBF) is responsible for the general research funding at the federal level. Overall, there is a regular intensive interaction between BMG and BMBF as well as with the other departments involved.
Research funding of Federal Ministry of Education and Research (BMBF)
The Federal Ministry of Education and Research (BMBF) is largely responsible for research among the federal departments. The BMBF is systematically promoting research activities on Long COVID or Post COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). This happens under the umbrella of the Federal Government’s framework program for health research. The focus of BMBF funding is on long-term effects that persist 12 weeks and longer after the Corona virus SARS-CoV-2 infection, the so-called Post COVID (for an exact definition, see the question “What is Long COVID and how is it different from Post COVID”).
On one summary page, the BMBF informs of its research funding as well as the funded projects.
In May of 2021, BMBF published a guideline for “Funding of research projects on late symptoms of COVID-19 (Long COVID)”. The objective of the guideline was to tap the knowledge and experiences around this illness available only locally to some extent and make them accessible for practical application as expeditiously as possible. To this end, 10 research associations are funded with a total of 6.5 million euros.
In addition, the BMBF is funding the development of a National Clinical Study Group (NKSG) of Post COVID syndrome and ME/CFS at the Charité – Universitätsmedizin Berlin with 10 million euros from October 2022 to presently end of 2024. This will develop a research platform. Clinical pilot studies are conducted on this platform with already approved drugs and medical devices for Post COVID and ME/CFS. All the studies are accompanied by a comprehensive program. The program should help in better understanding the disease mechanisms and potential biomarkers will be explored. Such biomarkers can be certain biochemical features that could be helpful in the diagnosis of Post COVID.
As a part of a revision notification of the “Hybrid interaction systems for maintenance of health even in exceptional situations” measure, the BMBF is providing 6 million euros for five projects to explore interactive technologies that can serve in the diagnosis of Post COVID or support healthcare.
Besides this, long-term population studies are funded, which also provide important insights. For example, the health status of people who contracted COVID-19 is monitored for a long term in the NAPKON cohorts (Patient groups of National Pandemic Cohorts Network) of the Network of Medical University (NUM). That should enable us to draw conclusions on the risk factors and disease mechanisms.
The long-term effects of a Corona virus infection are also examined in the excellent institutes for health research under various projects. The research institutes are mostly financed for the long term by BMBF. To name a few examples, the Helmholtz Centre for Infection Research (HZI), German Centre for Neurodegenerative Diseases (DZNE) or Berlin Institute of Health (BIH).
The BMBF also supports the joint projects IMMME – Understanding the immunological pathomechanisms of post-infection Chronic Fatigue Syndrome (ME/CFS) with around 2.2 million euros. The project researches ME/CFS after viral diseases. The support is provided as a part of a funding initiative for interdisciplinary collaborations that research the disease mechanisms. The project shall research the causes and mechanisms underlying the illness and connected with the immune system. In addition, the so-called biomarkers, which could serve to diagnose ME/CFS should be researched further. Besides this, the treatment options for ME/CFS should be further developed.
The BMBF has taken up the need for fundamental biomedical research in the area of ME/CFS with the funding guideline “Interdisciplinary networks for research on pathological mechanisms of ME/CFS” dated 1 September 2023. Funds of up to 15 million euros have been designated for this purpose. The networks selected as a part of the scientific peer review have started their work and will address the standardised collection of clinical data and biomaterials among other things.
Two other funding measures should raise the special potentials, arising from the digitalisation for Long/Post COVID research. The measures for funding new approaches of data analysis and data division in Long/Post COVID-19 research (funding of around 6 million euros) announced in September 2023 shall enable the interdisciplinary research groups to identify hitherto unknown correlations through joint analysis of data from different areas. The funding guideline on “Computational Life Sciences – Digital Method for Research on Post-Acute Infection Syndrome (PAIS)” published in November 2023, is promoting the development of new or improved AI-based methods and analysis tools for research on PAIS, which can also be caused by SARS-CoV-2.
Research funding of Federal Ministry of Health (BMG)
The Federal Ministry of Health (BMG) also supports the research on Long COVID. The goals are to better understand the disease and to record their frequency more accurately. Apart from that, an appropriate care should be ensured.
The BMG is funding the patient-oriented research on Long COVID as a part of a multi-year funding priority since the end of 2024 or rather the beginning of 2025. The focus of the funding is on 30 model projects, which will develop and test innovative forms of care for the treatment of COVID long haulers. The creation of a network shall stimulate information sharing, initiate patient care research, and thus improve the care to long haulers. The aim here is that research results for the treatment of Long COVID should come into patient care as soon as possible and vice versa, that the data from patient care should be available to the researchers. As a part of the multi-year funding priority for patient-oriented research on Long COVID, the BMG has a total of up to 81 million euros (2024 to 2028) at its disposal.
The BMG is also funding care measures especially for children and adolescents with Long COVID. Up to 52 million euros (2024 to 2028) are available for model projects on care of children and adolescents with Long COVID for the “Model measures for care of children and adolescents with Long COVID”. The aim is to create a network of special outpatient clinics with family doctors, paediatricians, and other service providers, which shall contribute considerably in improving patient care. A total of four projects are funded in this context. The projects selected for funding will start their work at the end of 2024 and in the beginning of 2025.
Both the funding priorities will consider ME/CFS specifically and throughout all stages. Illnesses with symptom complexes similar to Long COVID such as ME/CFS, even independent of a COVID-19 illness, and symptoms coinciding with a COVID-19 vaccine are also an object of research or shall also be considered in the projects.
Further research funding with the involvement of BMBF and BMG
In addition, research projects on “Post viral symptom complexes” such as Long COVID are funded through the innovation funds from the Joint Federal Committee (G-BA). In earlier research decisions of the Innovation Committee (2022 and 2023), projects on post viral symptom complexes had already been selected for funding with a total of around 11.4 million euros. Eight patient care research projects with a funding amount of around 10.9 million euros were selected for funding in 2024. Likewise, a project of the New forms of care, which implements, supplements, and scientifically evaluates a graded care in compliance with the corresponding G-BA guideline (LongCOV-RL) was included in funding. The subject was once again advertised in a funding announcement of June 2024 so that more projects can be funded.
Sources, BMBF-related:
https://www.mecfs.de/bmbf-foerdert-forschungsnetzwerk/
https://www.gesundheitsforschung-bmbf.de/de/13192.php
https://cfc.charite.de/klinische_studien/nksg/
https://www.bmbf.de/bmbf/shareddocs/bekanntmachungen/de/2020/10/3184_bekanntmachung
https://cfc.charite.de/weitere_forschung/immme/
https://www.gesundheitsforschung-bmbf.de/de/16423.php
https://www.gesundheitsforschung-bmbf.de/de/16755.php
https://www.gesundheitsforschung-bmbf.de/de/17113.php
Sources, BMG-related:
https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/lid/lid_node.html
https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Long-COVID/Projekt-Post-COVID.html
Sources, G-BA-related:
https://cfc.charite.de/klinische_studien/cfs_care/
Further information:
Last update: December 2024
Useful links
Information about Long COVID
- Information portal of the Robert Koch Institute (RKI) on Long COVID
- Post-COVID website of the Bavarian State Ministry of Health and Care (STMGP)
- Post-COVID website of the State Center for Health Promotion in Rhineland-Palatinate e.V. (LZG)
Search for medical practices and hospitals
- Hospital directory of the German Hospital Federation (DKG)
- Doctor search of patient service 116117 of the National Association of Statutory Health Insurance Physicians (KBV)
Dealing with Long COVID on a day-to-day basis
- Guideline ‘Long/post COVID syndrome’ for sufferers, relatives, loved ones and carers
- Information about pacing as a strategy for disease management from the German society for ME/CFS
- Consultation atlas of the supplementary independent participation consultation (EUTB
- Brochure about dealing with Long COVID symptoms of the World Health Organisation (WHO)
Communication with others
- Self-help group finder of Bundesarbeitsgemeinschaft Selbsthilfe von Menschen mit Behinderung, chronischer Erkrankung und ihren Angehörigen (Federal Association of Self-Help Organisations for people with disabilities and chronic diseases and their relatives) e.V. (BAG Selbsthilfe)
- Database and information on self-help groups on Long COVID in Germany from the National Contact and Information Centre for the Encouragement and Support of Self-Help Groups (NAKOS)
- Long COVID convention for specialists and affected persons of the doctors’ association for Long COVID
Information on ME/CFS
