Note: The following text is a guest article. They reflect the personal views of the author. The article is not an expression of opinion by the Federal Ministry of Health.
Guest article: Dr. Thomas G. Grobe, MPH
How common is Long COVID in Germany? An approximation based on routinely recorded data from health care
We define Long COVID as certain prolonged health impairments after a SARS-CoV-2 infection. Long COVID can have different symptoms and can vary in severity. The guest article by Dr Thomas G. Grobe addresses the question of how many people in Germany are affected by Long COVID.
Published on 08.09.2023.

© Copyright: Aqua
How common is Long COVID in Germany? An approximation based on routinely recorded data from health care
As with other infections, a SARS-CoV-2 infection can lead to prolonged health complaints and limitations. The severity of the symptoms can vary from person to person. While some of those affected are hardly restricted in their daily lives, others may find it impossible to carry out even the most routine tasks. If a connection with a previous SARS-CoV-2 infection is assumed, both cases can be referred to as Long COVID. This guest article attempts to provide insights into the symptoms and frequency of Long COVID based on analyses of data routinely available from health insurance companies. Essentially, the results presented below are based on two studies, which will be explained here as examples. Both studies were conducted on behalf of health insurance funds at the aQua-Institute and published in the year 2022. In addition, more recent estimates on the significance of Long COVID are also explained at the end of the article. Under certain conditions, routinely recorded data could provide more comprehensive and, in particular, faster information in situations such as the coronal pandemic in the future.
Advantages and disadvantages of routinely recorded data
An essential methodological advantage of having routinely recorded data, as is the case with health insurance funds, is that they are continuously documented in the context of health care. Thus, in addition to statements on the development of health in the course of the pandemic, statements on health before the corona pandemic are also attainable with the data, which were documented independently of subsequent events. In the case of Long COVID, this is relevant in order to assess frequencies of health complaints even before a SARS-CoV-2 infection. In addition, routinely recorded data analyses can often draw on data on very large populations of several million people. Studies with separate surveys on a corresponding scale would be impractical and simply unaffordable.
A disadvantage here may be that, as a rule, only information relevant to billing or reimbursement is logged in the routinely recorded data. If due to certain complaints no doctor is contacted or if the complaints are considered less relevant, then they inevitably do not appear in the routinely recorded data. Moreover, since diseases and complaints are largely recorded in the data exclusively in the form of diagnosis codes, only diseases and complaints for which a corresponding diagnosis code exists can be documented. Furthermore, it should be noted that significant parts of the billing data have only been available for evaluation so far with a delay. Data on outpatient (panel doctor) care can typically only be accessed more than six months after the end of a billing quarter. The only data available from health insurance funds almost on a daily basis is that on sick leave, following the now largely complete implementation of the electronic certificate of incapacity for work (eAU) since 2023.
Health complaints in the temporal environment of SARS-CoV-2 infections
At the beginning of the corona pandemic, the focus was initially on the acute consequences of SARS-CoV-2 infections and questions about the spread of infection and its containment. Within the first months after the outbreak of the pandemic, it was inevitably only possible to speculate about the medium- to more long-term consequences of the infections with more mild and acute symptoms of the disease. The fact that survivors of severe COVID-19 illnesses, for example after prolonged ventilation, can still suffer from health restrictions for months after being discharged from hospital was - like in the case of all severe illnesses - to be expected.
The term Long COVID in the sense of persistent complaints, possibly also after a more mild and acute COVID-19 illness, was probably used by those affected by the disease from the United States as early as May of 2020. Subsequently, this name became established along with a number of other terms with partly different delimitations in detail. Within the diagnosis classification prescribed in Germany for the documentation of diseases in health care billing data (International Statistical Classification of Diseases and Related Health Problems, German Modification; ICD-10-GM), it has been possible since mid-November 2020 to also explicitly document Long COVID as "Post-COVID-19 condition, not further specified" (in the beginning for a short time in 2020 indicated by the ICD-10 code U07. 4!, then from 2021 with the code U09.9! and the superordinate code U09, "Post-COVID-19 condition").
Due to their continuous recording and documentation of all diagnoses considered relevant, the routinely recorded data is comparatively well suited for an explorative and open-ended search for conspicuous accumulations of complaints and illnesses over time after events such as SARS-CoV-2 infections, even without prior definition of assumptions. Based on data concerning the health care of more than 8 million insured persons in BARMER, gender-, age- and residence-standardised frequencies of documented diagnoses from outpatient and inpatient health care were determined against this background, both in the second half of 2019 and in the second half of 2020, in which the coding of a long-COVID diagnosis had not yet been established. From this population, n = 35,642 people had already been infected with the SARS-CoV-2 virus in the first half of 2020 (people infected for the first time in the second half of 2020 were not included in the analyses). It was then determined for the second half of 2019 and 2020 whether diagnosis rates among those infected in the meantime in the first half of 2020 deviated from the rates expected on the basis of their gender and age structure according to data on the total population in the respective half of the year. Results for the second half of 2019 with ratios greater than one indicate a diagnosis-associated increased risk of subsequent COVID 19 disease. In contrast, results with ratios greater than one as of the second half of 2020 indicate a more frequent occurrence of diagnoses over time after a first COVID 19 diagnosis, which can be interpreted as a first indication of the possible significance of the diagnosis as a sequelae of a preceding COVID 19 disease. However, clusters of diagnoses in the course of time after a COVID-19 disease can only be interpreted as possible symptoms of Long COVID if their clustering in the course of time after the COVID-19 disease is more pronounced than in the run-up to the disease. It is only if the quotients in the second half of 2020 are greater than in the second half of 2019 that there are indications for an interpretation as sequelae of the SARS-CoV-2 infection documented in the first half of 2020 with regard to the respective diagnosis considered.
Diagnoses documented more frequently after SARS-CoV-2 infections
Significant rises in the relative frequency of diagnoses in the second half of 2020 as compared to 2019 after a COVID-19 disease - by a factor of more than 2 - can only be seen in the following diagnoses after evaluations that take into account all diagnoses at different levels of the ICD-10 classification:
- "Other myopathies" (ICD-10 code G72, changes in 2020 versus 2019 by a factor of 2.1), including "Other myopathies described in more detail" (G72.8; factor 7.6)
- "Chronic fatigue syndrome" (G93.3, factor 2.8)
- "Viral pneumonia, not classified elsewhere" (J12, factor 9.2)
- "Adult respiratory distress syndrome [ARDS]" (J80.0, factor 9.3)
- "Telogen effluvium" (L65.0 - a specific form of hair loss, factor 4.0)
- "Olfactory and gustatory disorders" (R43, factor 3.8), including "Anosmia" (R43.0, factor 4.6), "Parosmia" (R43.1, factor 8.8), "Parageusia" (R43.2, factor 4.0) and "Other and unspecified olfactory and gustatory disorders" (R43.8, factor 4.0)
- "Infection following surgery, not classified elsewhere" (T81.4, factor 2.2)
- "Germ carrier of other infectious diseases" (Z22.8, factor 3.2)
These results show that, in addition to diagnoses that indicate (the persistence of) infections, myopathies, chronic fatigue syndrome, ARDS, forms of hair loss and, in particular, disorders of the sense of smell and taste in various forms are documented much more frequently after a COVID-19 infection than could be statistically expected. The purely empirical approach chosen here thus identifies a number of frequently discussed longer-term consequences of SARS-CoV-2 infection. If the data used had been available very promptly, corresponding evaluations would have been feasible as early as the beginning of 2021 and thereby prior to the establishment of a long-COVID diagnosis in medical practice.
At the same time, the evaluations revealed indications that many diagnoses are documented more frequently in previously SARS-CoV-2 infected persons than expected depending on gender and age, but that this also applies equally to comparative periods before the SARS-CoV-2 infection, which means that corresponding diagnoses can be considered as risk factors rather than as consequences of SARS-CoV-2 infections. This is especially true for a number of diagnoses from the ICD-10 chapter of mental disorders.
COVID-19 in 2020 - Sick leave with long COVID diagnosis in 2021
The proportion of people with sick leave with an explicit mention of a long-COVID diagnosis "Post-COVID-19 condition, unspecified" (ICD-10 code U09.9) in 2021 was determined within the framework of a further study with routinely recorded data based on data from the Techniker Krankenkasse (TK), which is presented here as an example. Within the framework of these evaluations, it was possible to take into account data concerning n = 4,278,610 persons aged 15 to 64 years who, in all three years from 2019 to 2021, would also have been obligated to submit a certificate of incapacity for work in the event that they were incapacitated for work due to illness, which is primarily the case for employees subject to social insurance contributions, and then as a rule for incapacities for work lasting more than three days. The required data on incapacity to work until the end of 2021 was, unlike diagnoses from outpatient care, already available for evaluations from February 2022. The focus of the evaluations on incapacity to work or sick leave also has the effect that only complaints in the sense of Long COVID with more serious health restrictions were taken into account - namely those that individually prevent the practice of the previous occupation.
Of the 4.3 million persons considered, n = 99,890 persons were affected by a COVID-19 infection with virus detection within 2020, i.e. in the first year of the coronal pandemic, according to available data on outpatient and inpatient care. Of these persons who, according to the data, were already demonstrably infected in the year 2020, n = 773 persons were reported to be incapacitated for work for at least a short time with a long COVID diagnosis in the following year, which corresponds to a share of 0.8 percent in relation to the previously infected persons. With an average of 105 days reported, the extremely long periods of absence from work among those affected with an incapacity to work with a long-COVID diagnosis were quite remarkable. For comparatively small subgroups among those affected by COVID-19, namely those with longer-term incapacity to work due to COVID-19 infections or longer hospital treatment with a COVID-19 diagnosis in 2020, even significantly higher risks for sick leave with a long-COVID diagnosis and, if applicable, then average periods of incapacity to work in the following year 2021 could be determined noticeably above 150 days. In the following year, people referred to ventilation in connection with COVID-19 were involved in about 10 percent of sick leaves associated with a long COVID diagnosis and then, if necessary, over a period of 190 days on average.
Current frequency(ies) of diagnosed long-COVID disorders
There are now also more up-to-date results from routine evaluations of data from health insurance companies. While within the year 2021, according to population-related standardised results based on data from BARMER, the diagnosis U09, "post-COVID-19 condition", was documented in outpatient care for about 0.54 per cent of the population, which corresponds to about 453,000 affected persons in Germany, the diagnosis was documented at least as a suspected diagnosis in 1.50 per cent of the population in 2022, which corresponds to about 1.26 million affected persons in 2022. However, no differentiation according to the degree of individual health restrictions can be made here on the basis of the information on the diagnosis alone.
Prevalence of long-COVID diagnoses by gender and age groups in 2022
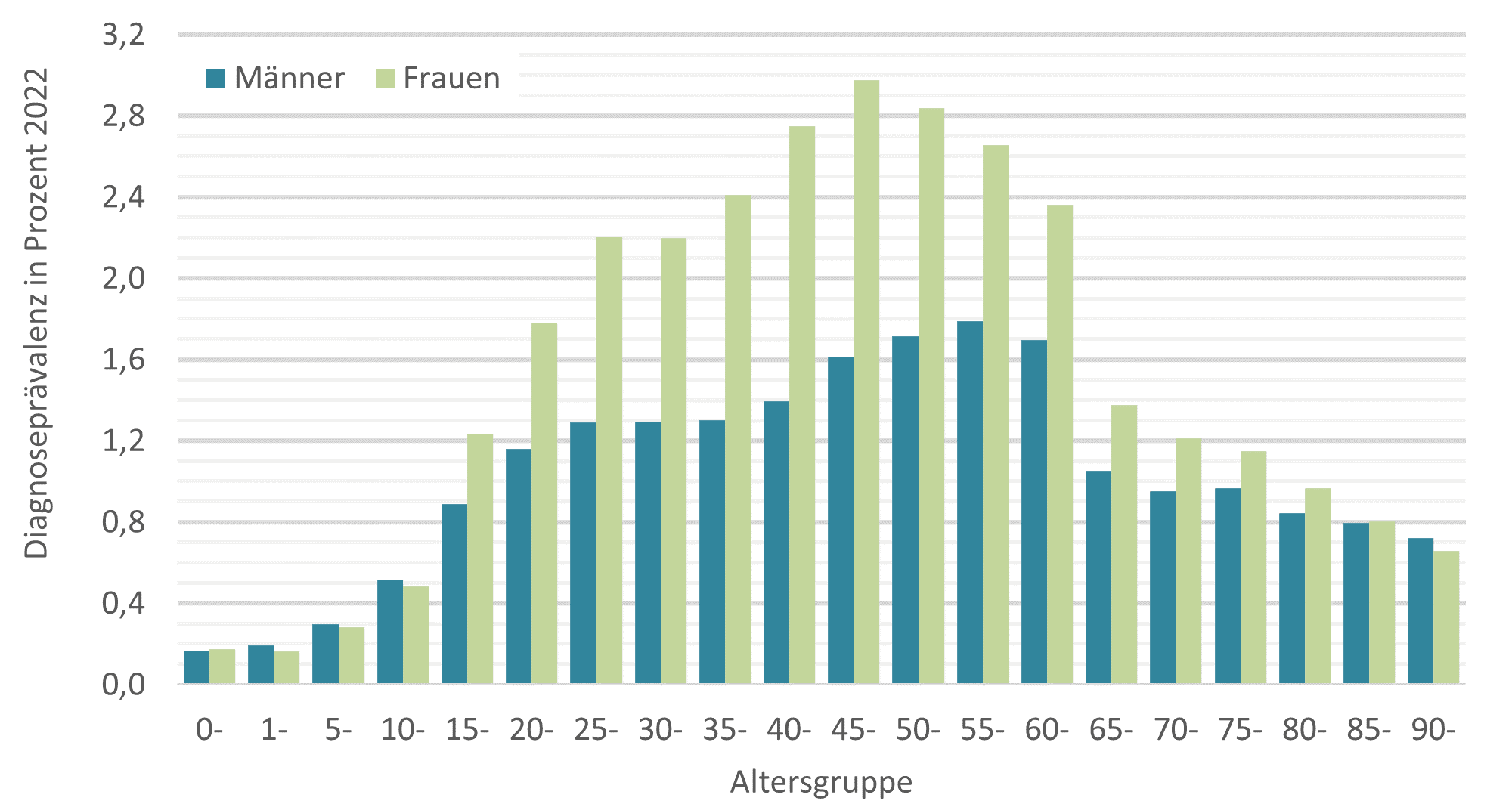
© Source: BARMER data 2022 on n = 8,643,122 insured persons, in-house calculation and presentation, persons affected with diagnosis U09, "post-COVID-19 condition", within the framework of outpatient medical and psychotherapeutic care without taking exclusion diagnoses into account, weighted where appropriate according to population structure in Germany as of 31.12.2022, differentiated according to gender, age groups and federal states according to information from the Federal Statistical Office.
The diagnosis U09 could be held accountable for a sickness rate of 0.013 per cent in the labour force within the year 2021, according to data from the Techniker Krankenkasse. It was subsequently found to be responsible for a sickness rate of 0.031 per cent in 2022. While the values at the beginning of 2023 were at a similar level as in the second half of 2022, preliminary data from May to July 2023 showed values below 0.03 per cent, and thus sickness rates could also be determined slightly below the previous year's results. A sickness rate of 0.03 per cent corresponds to the statement that 0.03 per cent of all employees - and thus one in every 3,333 employees - were reported unfit for work due to Long COVID on all days in the respective period under consideration. In the year 2022, about 0.6 per cent of all reported days of absence from work among TK-insured employees were attributable to the diagnosis U09 or Long COVID.
Sickness absences with long-COVID diagnosis as a weekly average in the years from 2020 to July 2023
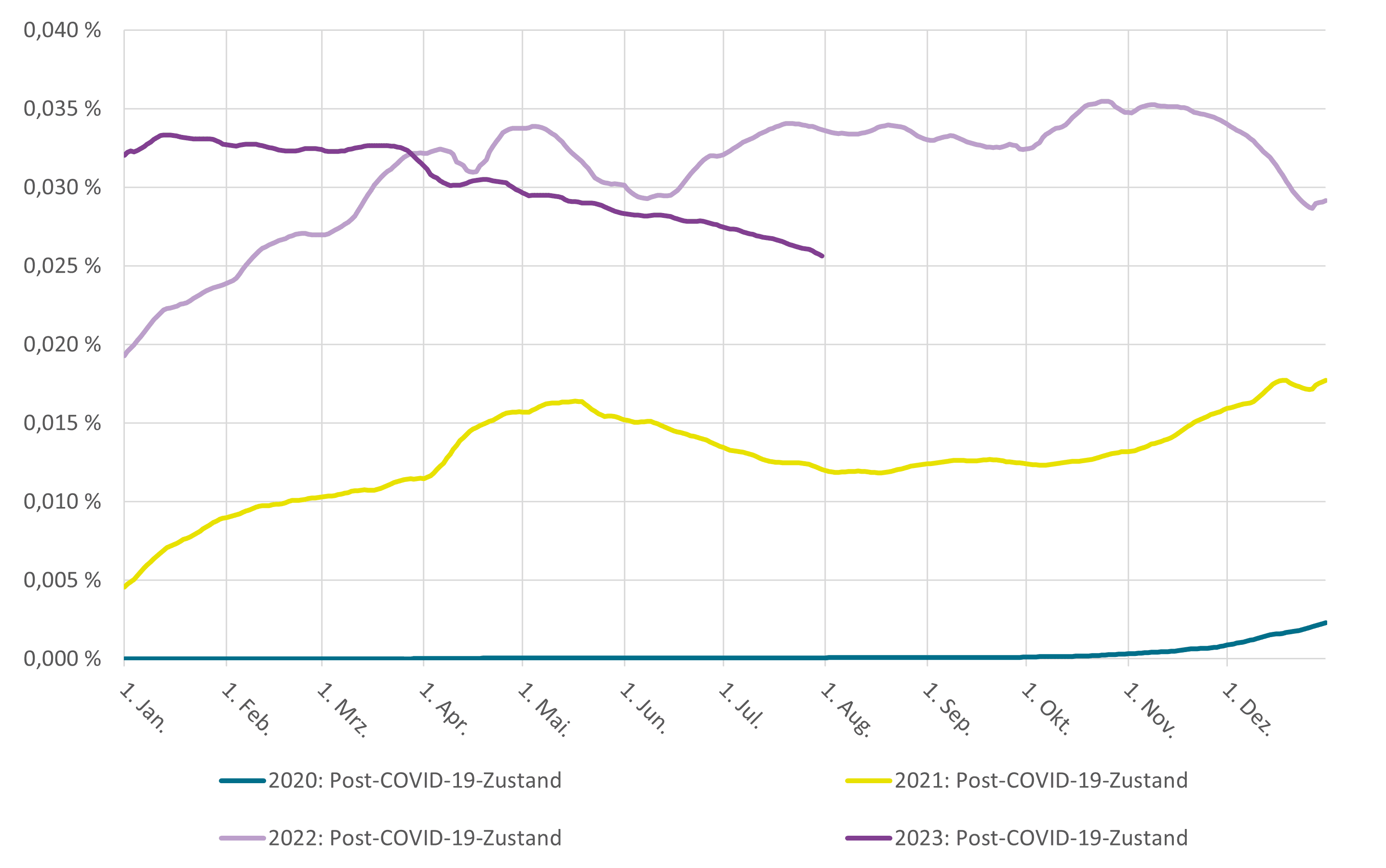
© Source: In-house calculations for the health report of Techniker Krankenkasse with data as of August 2023; reported incapacity to work with ICD-10 diagnosis U09, "post-COVID-19 condition", with daily n = 5,294,451 to n = 5,646,050 Working population insured with TK aged 15 to 64, daily values for sickness absence uniformly standardised according to the gender and age structure of the working population in Germany in 2010 according to data from the Federal Statistical Office; results for 2023 provisional - subsequent reports of cases of illness are to be expected to a limited extent.
Summary
As the study specimens presented here indicate, routinely recorded data from statutory health insurance funds potentially enables a multitude of analyses on health-related topics. With the Forschungsdatenzentrum (FDZ) (Research Data Centre) at the Bundesinstitut für Arzneimittel und Medizinprodukte (BfArM) (Federal Institute for Drugs and Medical Devices), it will also be possible in the future to conduct analyses with data from other health insurance funds. However, population-based estimates of the prevalence and significance of diseases are in many cases already achievable with data from individual health insurance funds.
Unlike the situation with many other health-related topics, in the course of the corona pandemic there emerged a need for information that should be satisfied at very short notice and as quickly as possible. In this context, an accelerated availability of data would also have been much appreciated for analyses of routinely recorded data. In the meantime, we are seeing advances towards data that is also available very quickly in practice, thanks to the extensive implementation of the eAU in particular.
Despite the rather low SARS-CoV-2 infection figures in Germany during the first wave of the corona pandemic in 2020, it was already possible to make estimates of the medium-term effects of corresponding infections in the sense of Long COVID with data for this year.
In 2021, Long COVID was estimated to have been diagnosed in around 450,000 people in Germany; in 2022, more than 1.2 million people were affected, women more frequently than men, and with the highest rates of affected people in the middle age group around 50 years. Long COVID is therefore by no means a rarely diagnosed disease in Germany. It is difficult to estimate the extent to which these figures are influenced by under- or possibly over-reporting. Since Long COVID can have very different symptoms, a differentiation of restrictions in daily life, which is already conceivable in the context of diagnosis coding, would contribute to a better assessment of the significance of documented diagnoses.
In the following year, "only" about one in a hundred of the SARS-CoV-2-infected employees in 2020 who were insured with TK declared themselves unfit for work with an explicit mention of a long-COVID diagnosis. However, those affected were then registered as unfit for work for an exceptionally long period of time in 2021. Sick leave in 2022 was also considerably higher than in 2021. Even if current figures on the course so far in 2023 cannot yet be considered complete, it seems to be evident that there will not be another sharp spike this year. The figures on reported incapacities to work suggest - despite various limitations - that Long COVID in Germany will not lead to a very serious loss of manpower as far as the national economy is concerned, at least for the time being. On the other hand, the figures also clearly show that there are a number of people whose lives are significantly affected by Long COVID.
Vita
Dr. med. Thomas G. Grobe, MPH, studied medicine and public health in Hanover. Since the year 2013, he has been working at the aQua Institute in Göttingen, where he heads the Department of Health Reporting and Biometry. Among other things, his department is currently working on more than ten research projects - often in cooperation with universities and other institutions - that are funded by the Innovation Fund. He has been involved with analyses of routinely recorded data from the area of statutory health insurance (SHI) since 1996. Under his direction, more than 50 health and physician reports with analyses, especially on incapacity to work and outpatient care, but also with cross-sectoral analyses on the basis of SHI routinely recorded data on very different topics, have been and are being published regularly since 1998 and/or 2006.
